Most people drink coffee without thinking twice. But if you’re taking medication, that morning cup could be quietly messing with your treatment-sometimes with serious consequences. Caffeine isn’t just a pick-me-up. It’s a powerful chemical that interacts with dozens of common drugs, changing how they work, how long they last, or even whether they work at all. And most people have no idea.
How Caffeine Interferes with Your Medications
Caffeine doesn’t just stimulate your brain. It also messes with your liver’s ability to break down drugs. The enzyme CYP1A2 handles about 10% of all prescription medications, and caffeine blocks it. That means drugs stick around longer in your body, building up to dangerous levels. It also interferes with how your gut absorbs some pills, making them less effective.
Think of it like this: your body is a factory. Medications are products moving through assembly lines. Caffeine is a worker who shows up late, knocks over tools, and redirects trucks. The result? Some products never get made. Others pile up and cause a backup.
High-Risk Interactions You Can’t Ignore
Not all interactions are created equal. Some are mild. Others can land you in the ER. Here are the top five you need to know about.
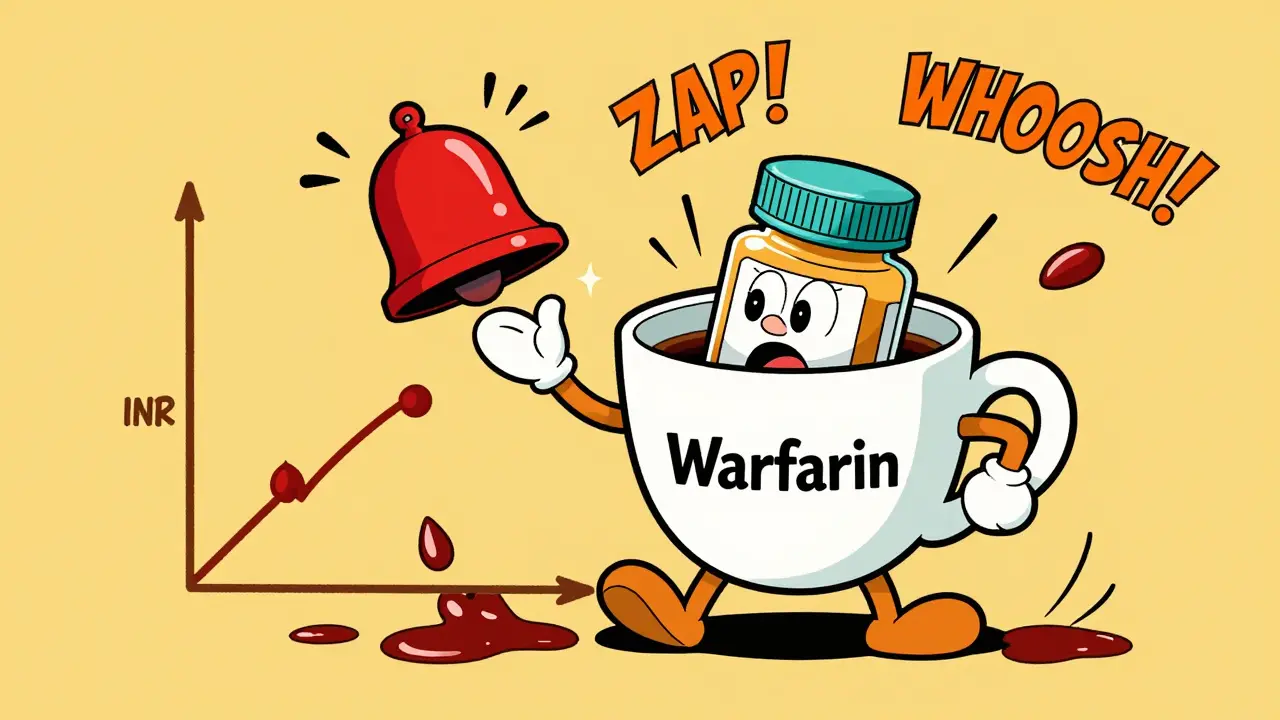
Warfarin and Caffeine: The Bleeding Risk
Warfarin (Coumadin) is a blood thinner used to prevent strokes and clots. It’s tricky to balance. Too little, and you clot. Too much, and you bleed. Caffeine makes it harder to keep that balance. When you drink coffee, caffeine slows down how fast your body clears warfarin. That can push your INR (a blood test that measures clotting time) up by 15-25% within 24 hours. One study found that 41% of people on warfarin who drank more than 200 mg of caffeine daily had INR levels above 4.0-well into the danger zone. Some needed emergency care for bleeding.
The FDA says you must keep your caffeine intake consistent. No sudden spikes. If you normally drink one cup a day, don’t switch to four. If you don’t drink coffee, don’t start-especially if you’re on warfarin.
Levothyroxine and Coffee: The Thyroid Trap
Levothyroxine replaces thyroid hormone for people with hypothyroidism. It’s absorbed in the upper intestine. Coffee, even black coffee, binds to it like glue. Studies show coffee can reduce absorption by up to 55%. That means your body gets barely half the dose you took.
One patient on Reddit, 'ThyroidWarrior2023,' took levothyroxine with coffee for three weeks. Her TSH-her thyroid hormone level-jumped from 1.8 to 8.7. That’s a massive shift. Her endocrinologist confirmed it: coffee was the culprit. The American Thyroid Association now recommends waiting at least 60 minutes after taking levothyroxine before drinking coffee. Some doctors suggest taking it first thing in the morning, then waiting until after breakfast to have your cup.
Antidepressants: When Caffeine Kills the Calm
SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) are common antidepressants. But caffeine can reduce their absorption by about 33%, according to Harvard Health. That doesn’t mean you’re not getting any help-but you might not be getting enough. People report feeling more anxious, jittery, or emotionally flat despite sticking to their dose.
On Drugs.com, over 1,200 users reported caffeine-antidepressant issues. Sixty-three percent said their anxiety got worse. Twenty-eight percent said their medication stopped working as well. It’s not always obvious. You might think you’re just stressed. But it could be your coffee.
One exception: bupropion (Wellbutrin). No significant interaction. But if you’re on any other SSRI, treat caffeine like a silent saboteur.
Theophylline and Caffeine: A Dangerous Duo
Theophylline is an old asthma medication. It’s rarely used now, but some patients still take it. The problem? Caffeine and theophylline are chemical cousins. They both use the same liver enzyme (CYP1A2) to break down. When you drink caffeine, theophylline builds up in your blood. Levels can rise 15-20%. That sounds small-but it’s enough to cause nausea, rapid heartbeat, tremors, or even seizures.
University Hospitals’ 2025 guidelines say asthma patients on theophylline should limit caffeine to less than 100 mg per day-about one small coffee. And watch for heart rates over 100 bpm. That’s a red flag.
Cardiac Stress Tests: Caffeine Can Fake a Heart Attack
Adenosine and dipyridamole are drugs used during stress tests to check for heart disease. They work by slowing your heart rate temporarily. But caffeine blocks their action. If you drink coffee, tea, soda, or energy drinks within 24 hours before your test, the drugs can lose 70-90% of their effectiveness. That means your test could come back normal-even if you have blocked arteries.
Doctors now require you to avoid all caffeine for 24 hours before a cardiac stress test. No exceptions. Not even decaf. Decaf coffee still has 5-15 mg of caffeine. That’s enough to ruin the test.
Other Dangerous Combinations
There are more than a dozen medications that react badly with caffeine. Here are a few you might not expect:
- Pseudoephedrine (Sudafed): Combined with caffeine, it can spike your heart rate by 20-30 beats per minute. That’s dangerous if you have high blood pressure or heart issues.
- Verapamil (Calan): A blood pressure pill. Coffee can reduce its effect by 25-30%. Take coffee at least two hours before or after this drug.
- Ephedrine: Found in some cold and weight-loss meds. With caffeine, it raises systolic blood pressure by over 30 mmHg in 68% of users. Risk of hypertensive crisis jumps 47%.
- Phenobarbital: Used for seizures. Caffeine can reduce its effectiveness and trigger breakthrough seizures.
Energy drinks are especially risky. They pack 80-300 mg of caffeine per serving-and add taurine, ginseng, and sugar. These ingredients can independently affect drug metabolism. One 2024 FDA report found that 68% of serious caffeine-medication incidents involved energy drinks, not coffee.
What You Should Do
Here’s what to do if you take any of these medications:
- Check your meds. Look at the label or ask your pharmacist. If it says 'avoid caffeine' or 'may interact with stimulants,' take it seriously.
- Track your intake. Write down how much caffeine you consume daily. A cup of coffee = 95-200 mg. Tea = 20-60 mg. Soda = 30-40 mg. Energy drink = 80-300 mg.
- Time it right. For levothyroxine: wait 60 minutes. For verapamil: wait two hours. For warfarin: keep intake consistent. Don’t start or stop coffee suddenly.
- Speak up. Tell every doctor and pharmacist you see that you drink caffeine. Don’t assume they’ll ask.
- Watch your symptoms. If your medication seems less effective-or you feel jittery, dizzy, or have an irregular heartbeat-caffeine could be the cause.
Why This Problem Is Growing
More people are taking more medications. More people are drinking more caffeine. In 2025, 85% of American adults consume caffeine daily. The global caffeine market hit $31.4 billion in 2024. And the FDA says adverse event reports linked to caffeine-drug interactions jumped 37% between 2020 and 2024.
Worse, 62% of patients don’t even know caffeine can interfere with their meds, even though 89% drink it daily. Pharmacists are now required to screen for 17 high-risk caffeine-drug combinations during medication reviews. Electronic health records are starting to flag these interactions automatically. But until that’s everywhere, you’re your own best defense.
What’s Next?
Scientists are now studying how your genes affect caffeine metabolism. Some people break down caffeine quickly. Others slow it down-making them more prone to interactions. A $4.7 million NIH study launched in January 2025 is tracking how genetic differences influence warfarin-caffeine risks across different ethnic groups.
By 2028, personalized caffeine guidance based on genetic testing could become standard. Until then, the safest move is simple: know your meds. Know your coffee. And don’t assume it’s harmless.
Can I drink coffee if I take warfarin?
You can, but you must keep your caffeine intake consistent. Sudden increases-like going from one cup a day to three-can raise your INR by 15-25%, increasing bleeding risk. Avoid energy drinks and large amounts of tea or soda. Talk to your doctor about your usual intake and get regular INR checks.
How long after taking levothyroxine should I wait to drink coffee?
Wait at least 60 minutes. Coffee can reduce levothyroxine absorption by up to 55% if taken together. Some experts recommend taking the pill first thing in the morning on an empty stomach, then waiting until after breakfast to have coffee. Consistency matters more than timing-stick to the same routine every day.
Does decaf coffee have caffeine?
Yes. Decaf coffee still contains 5-15 mg of caffeine per cup. That’s not enough to affect most people-but if you’re on a medication like theophylline, or preparing for a cardiac stress test, even that small amount can interfere. If your doctor says 'avoid all caffeine,' assume decaf counts.
Can caffeine make my antidepressant stop working?
It can reduce absorption of SSRIs like fluoxetine and sertraline by about 33%. That doesn’t mean they stop working entirely, but you may notice less improvement in mood or more anxiety. If you’ve been on your medication for months and suddenly feel worse, consider your caffeine intake. Try cutting back for two weeks and see if things improve.
Should I stop drinking coffee if I take multiple medications?
Not necessarily-but you should be cautious. People taking five or more daily medications are 3.2 times more likely to have a clinically significant caffeine interaction. If you’re on warfarin, thyroid meds, heart meds, or asthma drugs, talk to your pharmacist. They can check for specific interactions. Don’t quit coffee cold turkey unless advised. Just be mindful and consistent.
Final Thought
Caffeine is everywhere. But your meds are not. If you take any prescription or over-the-counter drug, caffeine isn’t just a beverage-it’s a variable in your treatment plan. Treat it like a drug. Because it is.





Andy Heinlein
January 1, 2026 AT 04:14Ann Romine
January 3, 2026 AT 00:04Austin Mac-Anabraba
January 4, 2026 AT 06:15Phoebe McKenzie
January 4, 2026 AT 19:18gerard najera
January 5, 2026 AT 01:59Stephen Gikuma
January 6, 2026 AT 13:34Bobby Collins
January 7, 2026 AT 05:06Layla Anna
January 7, 2026 AT 19:50Heather Josey
January 7, 2026 AT 22:07Olukayode Oguntulu
January 8, 2026 AT 07:26