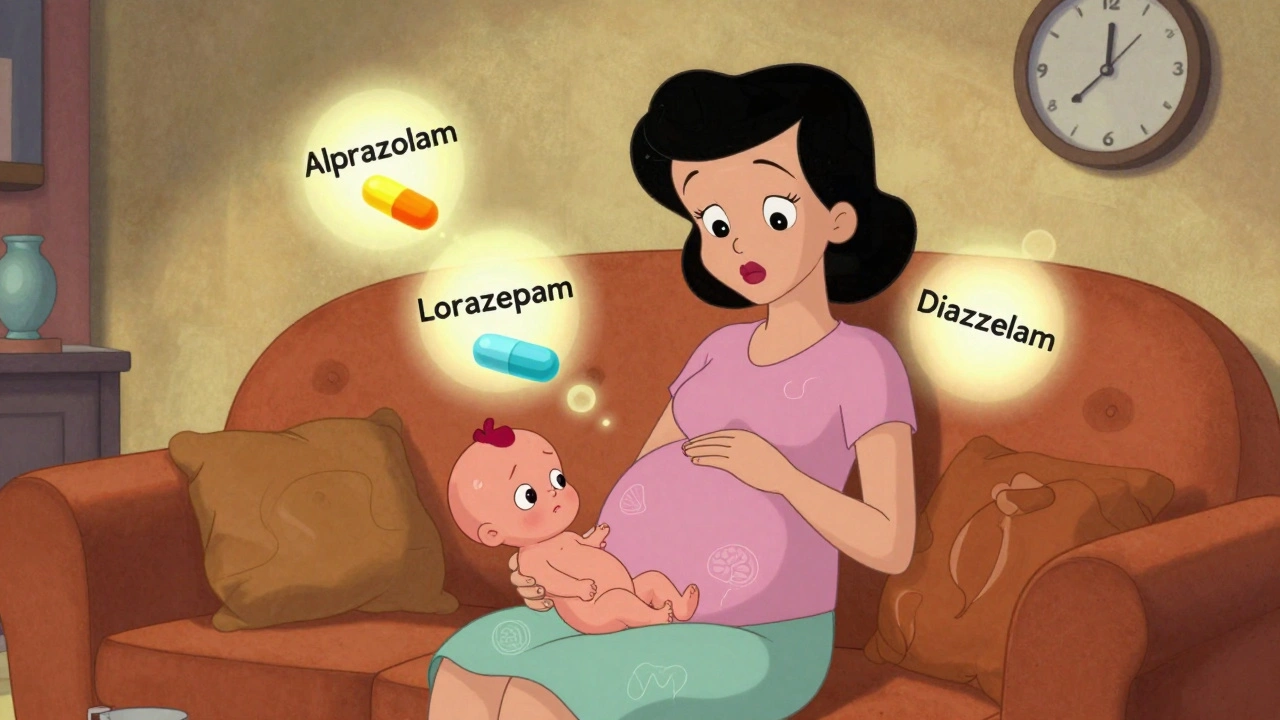
When you're pregnant and struggling with severe anxiety or insomnia, the pressure to feel better can be overwhelming. You might be told that benzodiazepines - drugs like alprazolam, lorazepam, or diazepam - are safe for short-term use. But what does the science really say about their risks to your baby? The answer isn’t simple, but it’s critical to understand before making any decisions.
What Are Benzodiazepines, and Why Are They Used in Pregnancy?
Benzodiazepines are a class of medications developed in the 1950s to calm the nervous system. They work by boosting the effect of GABA, a natural brain chemical that reduces nerve activity. That’s why they’re prescribed for anxiety, panic attacks, seizures, and sleep problems. About 1.7% of pregnant women in the U.S. get a benzodiazepine prescription during the first trimester, according to a 2024 JAMA Psychiatry study. Many of these women have conditions that haven’t responded to therapy or other medications.
But here’s the catch: benzodiazepines cross the placenta easily. Once they reach the developing fetus, they can build up in fetal tissue. That’s not just a theoretical concern - it’s been measured in studies. And because the baby’s liver and kidneys aren’t fully developed, they can’t clear these drugs the way an adult can. This means the baby is exposed longer and at higher concentrations than the mother might realize.
What Birth Defects Are Linked to Benzodiazepines?
The biggest fear for many pregnant women is birth defects. And while the overall risk is small, certain defects have shown up consistently in research.
A 2022 study in PLOS Medicine that tracked over 3 million pregnancies in South Korea found a small but real increase in overall birth defects - about 8 extra cases per 1,000 pregnancies exposed to benzodiazepines in the first trimester. The risk was even higher for heart defects: roughly 14 extra cases per 1,000 exposed pregnancies.
Other studies, like the CDC’s National Birth Defects Prevention Study, found stronger links to rare but serious defects:
- Dandy-Walker malformation - a rare brain structure problem - was nearly three times more likely with benzodiazepine exposure.
- Anophthalmia or microphthalmia (missing or underdeveloped eyes) was four times more likely with alprazolam use.
- Esophageal atresia (a blockage in the tube connecting the throat to the stomach) was nearly three times more likely with alprazolam.
- Pulmonary valve stenosis (a narrowed heart valve) was linked to lorazepam use.
These are rare conditions. The chance of any one of them happening is still low - maybe 1 in 1,000 or less. But when you’re pregnant, even a small increase in risk matters. And the data suggests that alprazolam carries higher risks than other benzodiazepines for certain defects.
Not All Studies Agree - Why the Confusion?
You might have heard that some studies found no link between benzodiazepines and birth defects. That’s true. A 2023 study in the British Journal of Clinical Pharmacology didn’t find a significant increase in major malformations. So why the contradiction?
The problem isn’t bad science - it’s confounding by indication. That’s a fancy way of saying: the reason you’re taking the drug might be the real cause of the problem. Women with severe anxiety or insomnia are more likely to smoke, have poor nutrition, miss prenatal visits, or experience high stress - all of which can affect fetal development. If you don’t account for these factors, you might wrongly blame the medication.
The 2022 PLOS Medicine study tackled this head-on. They used advanced statistical methods to control for these hidden factors. Even after adjusting for everything they could measure, the risk remained. That’s why many experts now believe the link is real, not just a statistical fluke.

Other Risks Beyond Birth Defects
Benzodiazepines don’t just affect how a baby is born - they can affect whether the pregnancy continues at all.
A 2024 JAMA Psychiatry study found that women who took benzodiazepines during pregnancy had an 85% higher risk of miscarriage. That’s a big jump. And it’s not just about the first trimester. Exposure in the 90 days before conception was also linked to a higher risk of ectopic pregnancy - a life-threatening condition where the embryo implants outside the uterus.
After birth, babies exposed to benzodiazepines in the womb are more likely to:
- Be born prematurely
- Have low birth weight
- Be small for their gestational age
- Have low Apgar scores (a measure of newborn health)
- Need time in the neonatal intensive care unit (NICU)
These aren’t minor issues. Premature birth and low birth weight are leading causes of infant health problems and long-term developmental delays. Even if your baby doesn’t have a birth defect, they could still face serious challenges after birth.
What’s the Real Risk? Numbers That Matter
It’s easy to get scared by headlines. But numbers help put things in perspective.
In unexposed pregnancies, about 2.87 out of every 100 babies are born with a major birth defect. In pregnancies where benzodiazepines were used, that number rises to 3.81 per 100. That’s an increase of 0.94 extra defects per 100 pregnancies - or about 1 in 100.
For heart defects specifically, the risk goes from about 1 in 200 to nearly 1 in 100. For alprazolam and eye defects, the risk jumps from less than 1 in 10,000 to about 1 in 2,500.
These aren’t huge numbers. But when you’re carrying a baby, even a 30% increase in risk isn’t something to ignore.
What Do Experts Say? Guidelines in 2025
Major medical groups are clear: benzodiazepines should be avoided in pregnancy - especially in the first trimester.
The American College of Obstetricians and Gynecologists (ACOG) says they can be used cautiously for short-term treatment, but only if no safer option exists. The American Psychiatric Association says decisions must be made case by case - considering the specific drug, dose, and timing.
Canada’s 2023 Clinical Practice Guidelines go further: they recommend avoiding benzodiazepines during pregnancy altogether, except in rare cases of severe, treatment-resistant anxiety where the benefits clearly outweigh the risks.
The FDA classifies benzodiazepines as Pregnancy Category D - meaning there’s clear evidence of fetal risk. The European Medicines Agency says avoid them in the first trimester unless absolutely necessary.
And here’s something important: alprazolam keeps showing up in the data as higher risk than other benzodiazepines. If you’re on alprazolam and pregnant, talk to your doctor about switching to a different medication - or better yet, a non-drug approach.
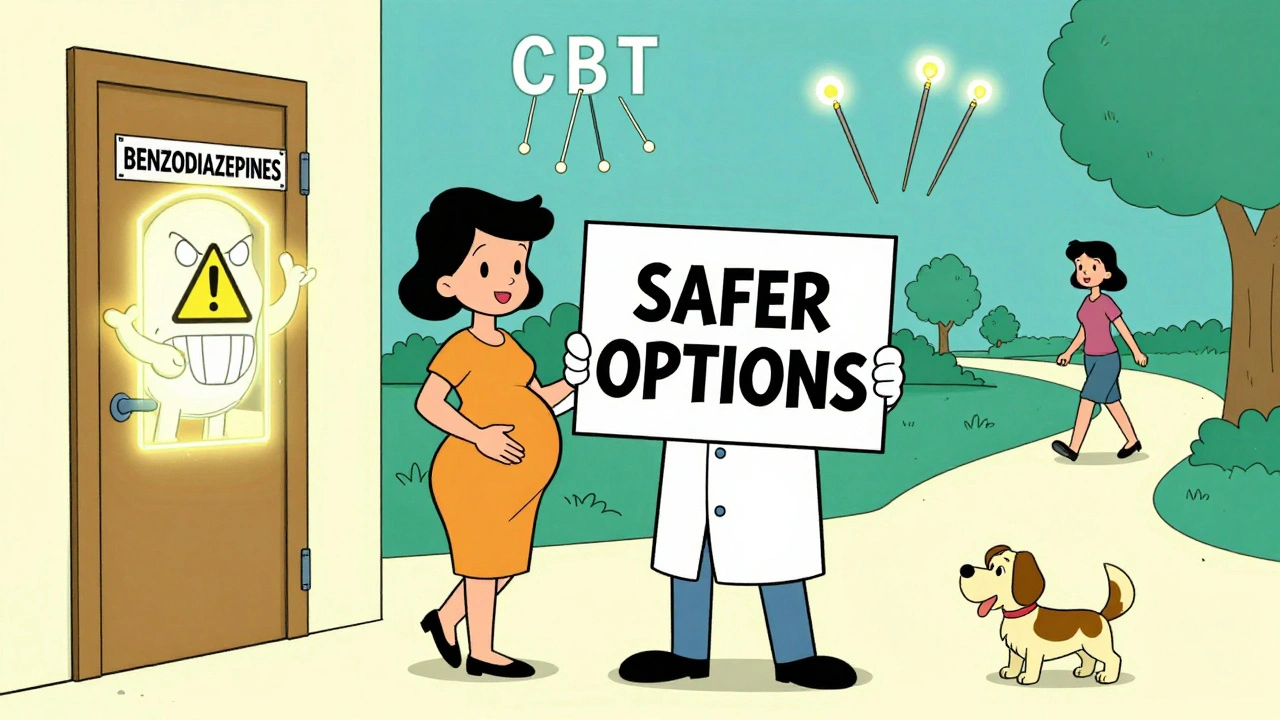
What Are the Alternatives?
You don’t have to suffer through anxiety or insomnia alone. There are safer options.
- Cognitive Behavioral Therapy (CBT) is the gold standard for anxiety and insomnia during pregnancy. It’s effective, doesn’t involve drugs, and works as well as medication for many women.
- Mindfulness and meditation have been shown to reduce anxiety and improve sleep quality in pregnant women.
- Exercise - even walking 30 minutes a day - can significantly lower anxiety and improve sleep.
- Acupuncture has been studied in pregnancy and shows promise for reducing anxiety and improving sleep without drugs.
- Non-benzodiazepine sleep aids like melatonin (in low doses) or certain antidepressants (like sertraline) may be safer alternatives - but only under medical supervision.
The key is to act early. Don’t wait until your anxiety is unbearable. Talk to your OB-GYN or a perinatal mental health specialist before you get pregnant, or as soon as you find out you’re expecting.
What If You’re Already Taking Benzodiazepines?
If you’re pregnant and currently taking a benzodiazepine, don’t stop cold turkey. Sudden withdrawal can be dangerous - for you and your baby. Seizures, severe anxiety, and even miscarriage can result from abrupt discontinuation.
Instead, make an appointment with your doctor. Bring your medication list. Ask:
- Is there a safer alternative for my condition?
- Can my dose be lowered gradually?
- Should I switch to a different benzodiazepine with lower risk (like clonazepam, which shows less association with defects)?
- Can I start therapy or other non-drug treatments alongside tapering?
Many women successfully transition off benzodiazepines during pregnancy with careful planning and support. You’re not alone, and you don’t have to power through this alone.
Final Thoughts: It’s About Informed Choice
No one wants to take medication during pregnancy. But sometimes, the cost of not treating severe anxiety or insomnia is higher than the risk of the drug. If you’re struggling, your mental health matters - for you and your baby.
The goal isn’t to scare you. It’s to give you the facts so you can make a decision that’s right for your body, your baby, and your life. Benzodiazepines aren’t safe for routine use in pregnancy. But they’re not a death sentence either. With the right support, most women can find a path forward that protects both their mental health and their baby’s development.



Audrey Crothers
December 12, 2025 AT 12:48OMG I was on Xanax when I got pregnant and I didn’t know!! 😭 My daughter is 2 now and she’s perfect but I still cry thinking about it. Talk to your dr, don’t panic, but don’t ignore this either. I wish someone had told me sooner.
Stacy Foster
December 13, 2025 AT 04:40They’re lying. The pharmaceutical companies paid off the researchers. Look at the CDC’s funding sources. They’re pushing this fear so you’ll take SSRIs instead - which are WAY worse for babies. The real cause? Vaccines. Or glyphosate. Or 5G. Pick one. But don’t trust the FDA - they’re in the pocket of Big Pharma.
Lawrence Armstrong
December 13, 2025 AT 23:24Just wanted to add - the PLOS Medicine study adjusted for smoking, stress, and prenatal care access. That’s huge. A lot of older papers didn’t. Also, clonazepam does seem safer than alprazolam in the data. Not zero risk, but better. And CBT? Life-changing. I did it during my second pregnancy after being on lorazepam. No meds, no guilt, better sleep. 🙌
Ashley Skipp
December 14, 2025 AT 10:05Why are we even talking about this like its a choice. If you’re anxious enough to need benzos you’re already a bad mom. Just suck it up and meditate. Or go for a walk. Everyone else manages. Your baby deserves better than your weak mind.
Nathan Fatal
December 16, 2025 AT 08:22There’s a deeper question here: what does it mean to be a responsible parent in a world where every choice carries risk? We’re told to avoid everything - caffeine, sushi, alcohol - but anxiety is invisible. Is it selfish to want peace? Or is it selfish to suffer in silence for a myth of purity? The data shows risk. But it doesn’t show suffering. And suffering has its own cost.
nikki yamashita
December 17, 2025 AT 00:50Y’all I just found out I’m 8 weeks and I’ve been on Klonopin for 5 years. I’m terrified but I’m calling my OB tomorrow. I’m not quitting cold turkey. I’m not feeling guilty. I’m just gonna do the next right thing. You got this. 💪
Adam Everitt
December 18, 2025 AT 14:16hmm… benzos and birth defects… i mean… maybe its not the drugs… maybe its the fact that people who take them are… like… more likely to be stressed out? or something? i dunno. the science is messy. also i think i spelled ‘benzodiazepine’ wrong. oops.
wendy b
December 19, 2025 AT 15:26It is, of course, imperative to acknowledge that the relative risk elevation, while statistically significant in certain cohorts, remains numerically modest in absolute terms. One must contextualize these findings within the broader epidemiological landscape of teratogenic exposure. Furthermore, the conflation of correlation with causation is a recurring fallacy in public health discourse. One would be remiss to overlook the confounding variables inherent in observational studies - particularly those involving self-reported medication adherence and psychosocial determinants of health. The suggestion that alprazolam is disproportionately hazardous lacks robust comparative pharmacokinetic analysis. One must proceed with intellectual rigor, not fear.