When you struggle to breathe, it’s not just about being out of shape. For millions with asthma or COPD, the problem is physical: airways tighten, swell, and fill with mucus. Two types of medications-bronchodilators and corticosteroids-are the frontline defense. They don’t cure the disease, but they make daily life possible. And understanding how they work, when to use them, and how to use them right can mean the difference between control and crisis.
How Bronchodilators Open Up Your Airways
Bronchodilators are the quick fix. Think of them as the emergency key that unlocks your airways when they’ve been locked shut. They don’t reduce swelling-that’s the job of corticosteroids. Instead, they relax the tight muscles wrapping around your breathing tubes.
There are two main types. Beta-2 agonists like albuterol (also called salbutamol) target receptors in your lungs, triggering a chemical chain reaction that tells muscles to loosen up. You feel the effect in 15 to 20 minutes, and it lasts 4 to 6 hours. That’s why it’s the go-to for sudden wheezing or shortness of breath. Long-acting versions like salmeterol or formoterol work the same way but last 12 hours or more. They’re not for emergencies. They’re for keeping things open all day.
The other type is anticholinergics-drugs like ipratropium and tiotropium. These block a different signal in your body that causes airways to constrict. They kick in around the same time as beta-2 agonists but work through a separate pathway. That’s why doctors sometimes combine them: more muscle relaxation, fewer side effects.
But here’s the catch: bronchodilators only treat the symptom, not the cause. If you’re using your rescue inhaler more than twice a week, something deeper is wrong. Overuse can lead to receptor fatigue-your body gets less responsive over time. Heavy users can lose up to half the benefit they once got.
How Corticosteroids Quiet the Inflammation
If bronchodilators are the key, corticosteroids are the peacekeepers. They don’t open your airways. They stop them from getting tight in the first place.
These are not the same as the steroids athletes abuse. Inhaled corticosteroids like fluticasone, budesonide, and mometasone work locally in your lungs. They slip into cells and turn down the volume on over 100 inflammatory genes. Less swelling. Less mucus. Less sensitivity to triggers like cold air, pollen, or smoke.
But they don’t work fast. You won’t feel better after one puff. It takes days-sometimes weeks-of consistent use before your lungs calm down. That’s why people often stop taking them. “I don’t feel anything,” they say. But if you skip doses, inflammation creeps back. And when it does, your airways become more reactive. You end up needing more rescue inhalers. It’s a vicious cycle.
Studies show regular use cuts asthma flare-ups by 30 to 60%. In COPD, it reduces hospital visits by nearly half. But it’s not magic. If you don’t use it daily, it’s useless. And if you use it without rinsing your mouth afterward, you risk oral thrush-a fungal infection that causes white patches and discomfort. That’s why rinsing isn’t optional. It’s part of the treatment.

Why They Work Better Together
Here’s the secret most people miss: bronchodilators and corticosteroids aren’t just used together-they need to be used in order.
Imagine trying to paint a wall with a thick brush while the door is shut. You can’t reach the corners. Now open the door. Suddenly, you can cover everything. That’s what bronchodilators do for corticosteroids. By relaxing the airways, they let the anti-inflammatory drug reach deeper into the small tubes where inflammation hides.
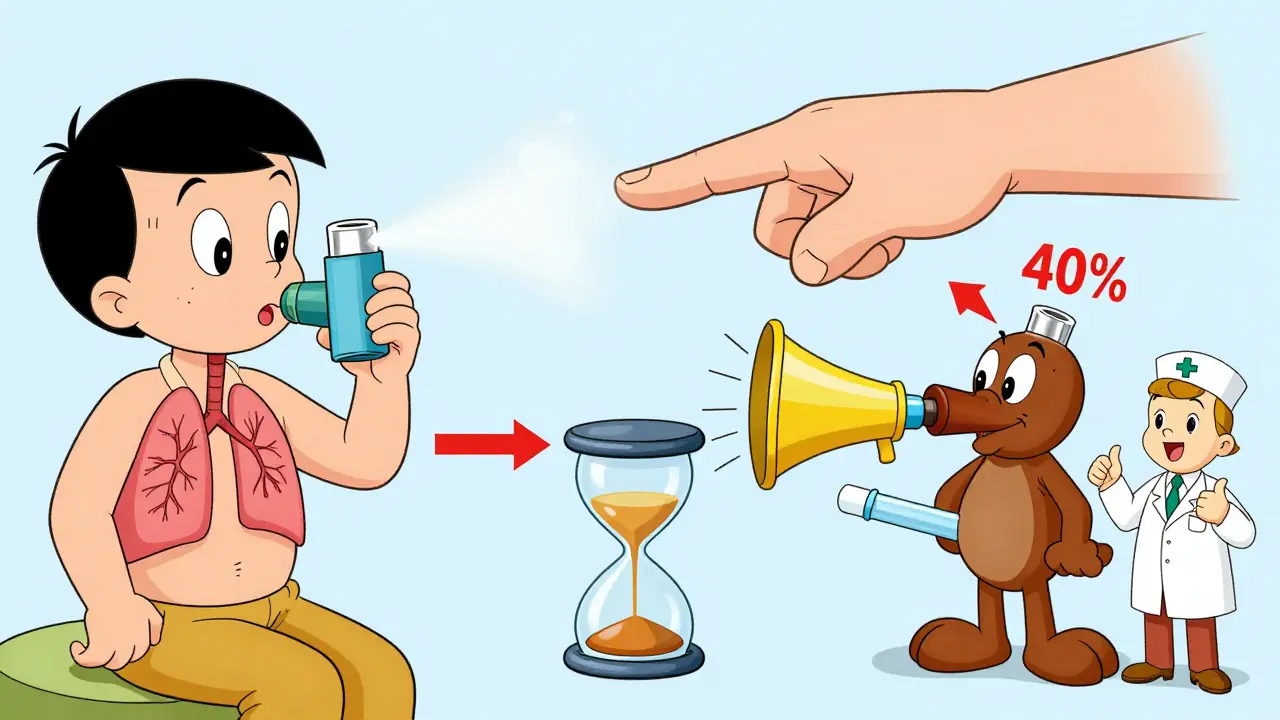
Experts agree: always use your bronchodilator first. Wait five minutes. Then use your corticosteroid. This simple sequence improves drug delivery by up to 40%, according to studies from the American Thoracic Society. Skip the wait, and most of the steroid just hits your throat and gets swallowed-wasted.
That’s why combination inhalers like Advair (fluticasone/salmeterol) and Symbicort (budesonide/formoterol) became so popular. They deliver both drugs in one device. But even then, timing matters. Symbicort is unique-it’s approved for both rescue and maintenance because formoterol works fast enough to act as a rescue inhaler while still delivering steroid. GINA 2023 now recommends this combo as the first choice for mild asthma, replacing the old standard of albuterol alone.
And now, there’s Airsupra-the first FDA-approved as-needed combo inhaler. It gives you both immediate relief and anti-inflammatory action in one puff. For many, this is a game-changer.
What Happens When You Use Them Wrong
Most people don’t know how to use their inhalers. A 2022 study found only 31% of patients use them correctly without training. That’s not because they’re careless-it’s because the devices are confusing.
There are metered-dose inhalers (MDIs), dry powder inhalers (DPIs), and nebulizers. Each requires different technique. MDIs need a slow, deep breath timed with a spray. DPIs need a fast, hard inhale to pull the powder in. Get it wrong, and less than 10% of the medicine reaches your lungs.
Spacers help. These plastic tubes attach to your inhaler and hold the medicine so you can breathe it in slowly. Studies show they boost lung delivery by 70%. They’re especially helpful for kids and older adults.
Another big mistake: mixing up rescue and maintenance inhalers. One is blue, one is brown. One is for when you’re struggling. The other is for every day, even when you feel fine. A 2022 survey found 44% of asthma patients couldn’t tell which was which. That’s dangerous. Using a steroid inhaler as a rescue drug won’t help your sudden attack. Using a rescue inhaler every day won’t stop the inflammation building up.
And then there’s the fear of steroids. Some people avoid them because they’ve heard about side effects. Yes, high doses over years can increase pneumonia risk in older COPD patients. Yes, they can cause hoarseness or thrush. But the risks of uncontrolled asthma-ER visits, missed work, ICU stays-are far worse. For most people, the benefits far outweigh the risks.
Real People, Real Results
On Reddit’s asthma community, users shared stories that mirror the science. One person said they used their rescue inhaler 10 times a day. After switching to a combination inhaler and learning to wait five minutes between puffs, their ER visits dropped from four a year to zero.
Another user, who’d been using a dry powder inhaler for years, realized they were breathing too slowly. After a 15-minute demo with a respiratory therapist, their lung function improved by 25% in just two weeks.
But the most common complaint? “My inhalers never worked well until my nurse showed me to use the blue one before the brown one.” That’s not a coincidence. It’s the sequence.
And the side effects? Tremors from albuterol? Hoarseness from steroids? Yes. But most people find them manageable. Rinsing your mouth, using a spacer, and tracking your usage with a simple journal makes a huge difference.
What’s Next for Respiratory Medications
The future is getting smarter. Doctors are now using FeNO tests-measuring nitric oxide in your breath-to see how much inflammation is present. That helps tailor steroid doses. No more guessing.
Triple-therapy inhalers-combining two bronchodilators and a steroid-are now available for severe COPD. Trelegy Ellipta, for example, cuts flare-ups by 25% compared to dual therapy.
And there’s growing pressure to make inhalers greener. A single albuterol inhaler has the carbon footprint of driving 300 miles. Dry powder inhalers, which don’t use propellants, now make up 45% of new releases since 2020. That’s a step forward.
But the biggest leap won’t come from a new drug. It’ll come from better education. When patients understand the difference between a rescue inhaler and a controller, when they know to wait five minutes, when they rinse their mouth and use a spacer-they stop flying by the seat of their pants. They start managing their disease.
Respiratory medications aren’t just pills or puffs. They’re tools. And like any tool, they only work if you know how to use them.



Bobbi-Marie Nova
January 18, 2026 AT 11:37OMG I used to think my brown inhaler was just a fancy air freshener. Then my nurse showed me the 5-minute rule and my life changed. I haven’t been to the ER in 2 years. Rinsing my mouth? Still gross, but worth it. 🙌
Joie Cregin
January 18, 2026 AT 12:32I used to skip my steroid inhaler because ‘I feel fine.’ Turns out, ‘feeling fine’ is just the calm before the storm. Now I take it like brushing my teeth-no drama, no excuses. My lungs thank me. Also, spacers are magic. Get one. Even if you think you’re too cool for it.
kanchan tiwari
January 18, 2026 AT 15:07They don’t want you to know this but the government secretly replaced all the albuterol with placebo pills so you’ll buy more combo inhalers. Big Pharma’s been pushing this ‘wait 5 minutes’ nonsense since 2018. My cousin in Delhi says his grandma still uses a nebulizer and she’s 92 and still hiking. Coincidence? I think not.
Corey Sawchuk
January 18, 2026 AT 18:22I used to mix up my inhalers too. Blue for panic, brown for boredom. Then I started labeling them with tape and a Sharpie. Simple. Dumb. Works. Also, rinsing after steroids? Yeah I do it. Don’t care if it’s annoying. Thrush is not a vibe.
Nick Cole
January 19, 2026 AT 01:19Let’s be real-most people don’t know how to use an inhaler. I’ve seen people shake it like a cocktail, spray into the air, then take a shallow puff. No wonder their meds don’t work. Training isn’t optional. It’s survival. If your doctor doesn’t show you how to use it, demand a demo. Or go to a pharmacist. They’ll actually help.
waneta rozwan
January 19, 2026 AT 06:02Oh honey. You think you’re the first person to figure out the 5-minute rule? I’ve been yelling this at my asthma group since 2015. And still-half the room uses the steroid first. Then wonders why they’re still wheezing. It’s like putting sunscreen on after you’re already sunburned. Do you see how that’s backwards? I’m not mad. I’m just disappointed.
And yes, Airsupra is a game-changer. But guess what? It still costs $500 if you don’t have insurance. So maybe we need to talk about that too. Not just the science. The system.
Also, I tried the dry powder inhaler. My 78-year-old mom nearly passed out trying to inhale fast enough. Spacers aren’t for kids. They’re for anyone who’s ever breathed.
Riya Katyal
January 19, 2026 AT 14:55Wait… so you’re telling me the blue inhaler isn’t just a ‘happy pill’? I thought it was for mood swings. My sister says her inhaler makes her feel ‘lighter’-like she’s floating. Maybe it’s not asthma. Maybe it’s just bad vibes.
Kasey Summerer
January 21, 2026 AT 14:51Bro I used to think the ‘brown’ inhaler was for allergies. Like, ‘oh I’m sneezing, time for brown.’ Then I realized it’s for the invisible war inside my lungs. Now I use it like a daily meditation. Breathe in. Hold. Breathe out. Rinse. Repeat. 🤫
Henry Ip
January 22, 2026 AT 14:05For real-don’t skip the rinse. I used to hate it. Thought it was overkill. Then I got thrush. White patches. Burning. Felt like my mouth was full of moldy bread. Took 3 weeks to clear. Now I rinse like I’m saying a prayer. And I use a spacer. It’s not embarrassing. It’s smart. You’re not weak for needing help. You’re just not stupid.
Nicholas Gabriel
January 22, 2026 AT 16:48Let me just say this: If you’re using your rescue inhaler more than twice a week, you’re not managing your asthma-you’re just surviving it. And if you’re not tracking your usage, you’re flying blind. Get a journal. Write it down. Date. Time. Puffs. How you felt before. How you felt after. It’s not therapy. It’s data. And data saves lives. Also, if you’re using a metered-dose inhaler without a spacer, you’re wasting over 90% of your medication. That’s like buying a $100 bottle of wine and only drinking the cork.
Jody Fahrenkrug
January 24, 2026 AT 16:25I used to think I was being lazy for needing two inhalers. Turns out I was just using them wrong. Now I keep them next to my toothbrush. Same routine. Same time. No thinking. Just doing. And yeah, the steroid makes my voice sound like a frog. But I’d rather sound like a frog than end up in the ER again.
Allen Davidson
January 25, 2026 AT 21:28My dad had COPD. He refused steroids because he thought they’d ‘weaken’ him. Then he got pneumonia, spent 3 weeks in the hospital, lost 20 pounds. After that, he started using his combo inhaler. Didn’t feel ‘better’-but he didn’t feel worse either. And that was enough. Sometimes managing chronic illness isn’t about feeling amazing. It’s about not crashing.
john Mccoskey
January 26, 2026 AT 19:16The entire paradigm of respiratory pharmacology is built on a foundation of corporate-sponsored placebo-controlled trials funded by companies that also manufacture the very devices patients are supposed to use correctly, which are themselves engineered with intentionally non-intuitive mechanisms that require manual dexterity most elderly patients lack, while simultaneously marketing these devices as ‘easy to use’-a blatant misrepresentation of human physiology and cognitive load, and the fact that the GINA guidelines now endorse combination therapy as first-line for mild asthma, despite the fact that the original RCTs were underpowered and excluded patients over 65 or with comorbidities, suggests that we are not treating disease-we are optimizing for market penetration under the guise of clinical advancement, and the real breakthrough isn’t Airsupra-it’s the fact that we still haven’t addressed the systemic failure of patient education in primary care, where the average consultation lasts 7 minutes and the only ‘training’ provided is a pamphlet printed in 6-point font with no diagrams and a QR code that leads to a login portal requiring a government-issued ID and three-factor authentication, which is frankly absurd in a country where 40% of adults can’t read above a 5th-grade level, and yet we expect them to master the precise timing of a metered-dose inhaler while simultaneously managing insulin, beta-blockers, and antidepressants, and then we wonder why compliance is below 30%-it’s not laziness, it’s a design flaw in the system, and until we stop blaming patients for failing to navigate a labyrinth built by pharmaceutical engineers who have never held an inhaler in trembling hands, we are not healing-we are merely selling.
Isabella Reid
January 27, 2026 AT 02:29My mom’s from India. She used to make her own herbal steam with eucalyptus and turmeric. Then she got a combo inhaler. She still does the steam. But now she also rinses. And uses the spacer. And doesn’t skip doses. She says, ‘Western medicine doesn’t replace tradition. It just gives it wings.’ I think that’s the best summary I’ve ever heard.