Most of the time, your pharmacist can swap a brand-name drug for a generic version without you even knowing it. It’s cheaper, just as effective, and approved by the FDA. But sometimes, your doctor writes a prescription that says "do not substitute" or "brand medically necessary". That’s not a mistake. It’s not laziness. It’s not because they’re being paid by the drug company - though that happens too. Sometimes, it’s because your health depends on it.
When a Generic Isn’t Enough
Not all drugs are created equal, even if they have the same active ingredient. For some medications, tiny differences in how the body absorbs the drug can mean the difference between control and crisis. These are called narrow therapeutic index (NTI) drugs. A small change in blood levels can lead to treatment failure or serious side effects. Drugs like levothyroxine (Synthroid) for thyroid conditions, warfarin (Coumadin) for blood thinning, and levetiracetam (Keppra) for epilepsy fall into this category. The American Thyroid Association recommends sticking with the same brand of levothyroxine because switching between generics - even ones approved by the FDA - has been linked to swings in thyroid hormone levels. One patient on Reddit shared that after switching from Synthroid to a generic, she developed severe depression and fatigue. When she went back to the brand, her symptoms vanished. A 2019 study in Epilepsy & Behavior followed 1,200 people with epilepsy who were switched from brand-name Keppra to a generic version. Over 12% had breakthrough seizures. Only 4.3% of those who stayed on the brand did. That’s not a small difference. For someone with seizures, that gap can mean hospital visits, injuries, or worse.Why the FDA Allows Generics - But Not Always
The FDA requires generics to be bioequivalent to brand-name drugs. That means they must deliver the same amount of active ingredient into the bloodstream within a range of 80% to 125%. Sounds tight, right? But for NTI drugs, that 45% range is wide enough to matter. Think of it like this: if you’re driving a car and need to stay exactly at 60 mph, a 10% variation might be fine. But if you’re flying a plane and need to maintain altitude within 5 feet, a 10% variation could be deadly. That’s what NTI drugs are like. The FDA itself acknowledges this. Their Orange Book lists drugs with therapeutic equivalence ratings. For NTI drugs, many are rated as “AB1” - meaning they’re considered equivalent - but experts still urge caution. That’s why many doctors, especially neurologists and endocrinologists, default to brand-name prescriptions for these drugs. It’s not about profit. It’s about predictability.It’s Not Just About the Active Ingredient
Generics have the same active ingredient, but they don’t have to match the brand’s inactive ingredients. That’s the filler, dye, coating, or binder that holds the pill together. For most people, these don’t matter. But for some, they do. Take ciprofloxacin, an antibiotic. One generic version might use a different coating than the brand. That coating can irritate the stomach. A patient might start having nausea, bloating, or diarrhea - not because the antibiotic isn’t working, but because their gut doesn’t tolerate the new filler. Switching back to the brand clears it up. Same goes for people with allergies. One generic might contain lactose. Another might use cornstarch. If you’re allergic to dairy, that small difference matters. Your doctor needs to know your history to pick the right version.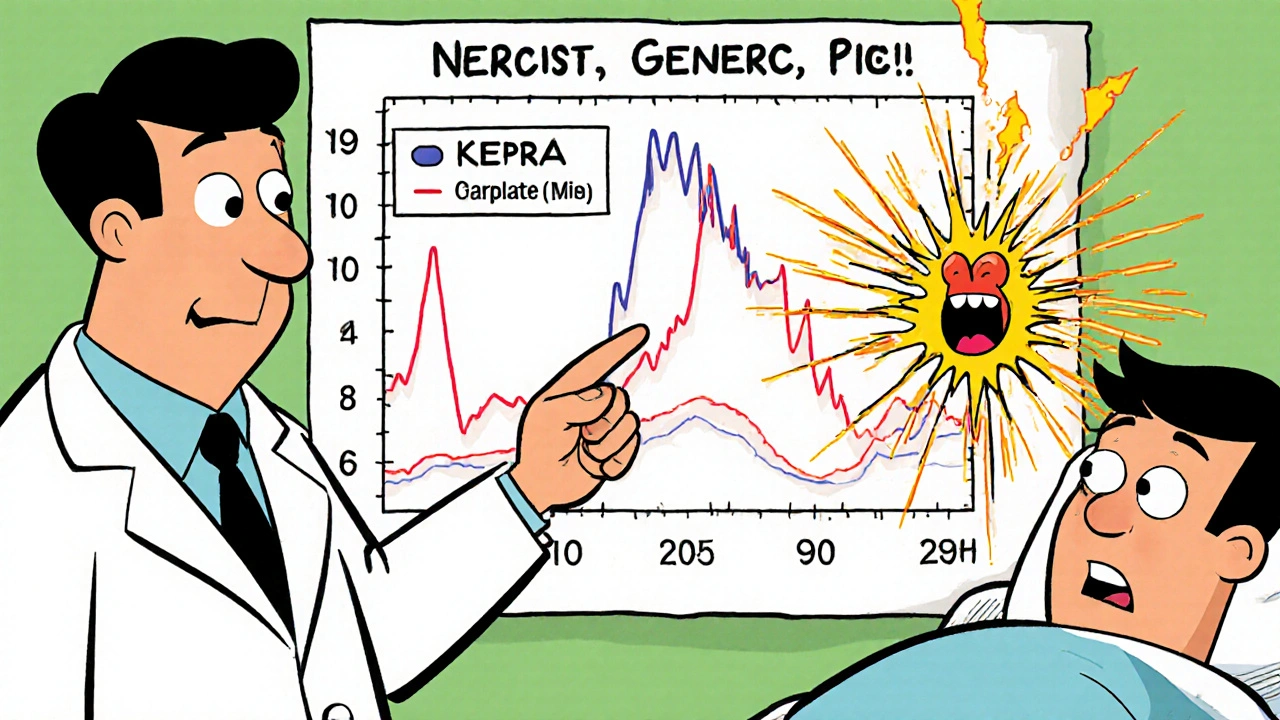
Insurance Doesn’t Always Make It Easy
If your doctor writes “brand medically necessary,” your insurance company doesn’t just automatically pay. They often require prior authorization. That means your doctor has to fill out paperwork explaining why the generic won’t work. The process can take 72 hours. Some insurers approve only 45% of requests for drugs like proton pump inhibitors, but 89% for antiepileptics - because they know the stakes are higher. And if the insurer denies it? You might pay hundreds more per month. One patient in a 2021 Kaiser Family Foundation survey said she paid $280 a month for her brand-name blood pressure drug - but the generic cost $15. She had to go to her doctor three times before they’d write the right prescription. That’s why some doctors avoid brand-name prescriptions unless absolutely necessary. They don’t want to put you through the hassle. But when it’s medically needed, they’ll fight for it.Most of the Time, Generics Are Perfect
Let’s be clear: for the vast majority of medications, generics are just as good. A 2020 JAMA Network Open review of 47 studies with over 112,000 patients found no difference in outcomes between brand and generic versions of statins, ACE inhibitors, antidepressants, and many others. GoodRx surveyed 15,328 people in 2022. Eighty-nine percent said their generic medications worked exactly like the brand. One man saved $1,200 a year switching from brand-name atorvastatin to the generic. He didn’t notice any difference in his cholesterol or energy levels. The numbers back this up: 90% of all prescriptions filled in the U.S. are generics. But they make up only 23% of total drug spending. That’s because brand-name drugs are expensive - often 80-85% more than their generic equivalents. A 2022 GoodRx report showed the average brand-name prescription cost $471.67. The generic? $13.76.Why Do Doctors Still Prescribe Brand-Name?
You might wonder: if generics are so effective and cheap, why do some doctors still prescribe brand-name drugs unnecessarily? Part of it is habit. Many doctors learned to prescribe by brand name during medical school. They say “Lipitor” instead of “atorvastatin.” That familiarity can lead to prescribing the brand, even when a generic exists. Drug reps also play a role. They visit doctors’ offices, hand out samples, and emphasize brand names. A 2018 study from Stanford found that when physicians use brand names in their notes, they’re more likely to prescribe the brand - even if they know the generic works. Patient demand matters too. Some people believe brand-name drugs are stronger or better. They’ve seen ads. They’ve heard stories. They ask for the name they recognize. Doctors, wanting to keep patients happy, sometimes comply - even when it’s not medically needed.
What You Can Do
If your doctor prescribes a brand-name drug, ask: “Is this medically necessary?” or “Is there a generic that would work just as well?” If you’ve had problems switching to a generic - like new side effects or loss of symptom control - tell your doctor. Bring your pharmacy receipt. Show them the difference in cost. Ask them to document it clearly on the prescription. Check your insurance plan. Some require you to try the generic first. Others have step therapy rules. Know your rights. Use the FDA’s Orange Book to look up your drug. Search for its therapeutic equivalence rating. If it’s rated “AB,” the generic is considered interchangeable. If it’s not, or if it’s an NTI drug, ask your doctor to explain why they’re choosing the brand.What’s Changing
The FDA is pushing for more consistency. In 2023, they issued new guidance asking generic manufacturers to match brand-name drugs in size, shape, and color - to reduce confusion and medication errors. That’s a big step. There’s also a rise in “authorized generics.” These are made by the original brand company but sold under a generic label. They’re identical to the brand - same ingredients, same factory - but cheaper. They’re not available for all drugs, but they’re growing. Biosimilars - generic versions of complex biologic drugs like Humira - are starting to enter the market. By 2027, they could capture up to 60% of that market, reducing the need for brand-only prescriptions. But until then, the system is still flawed. Too many people pay more than they should. Too many patients are switched without warning. Too many doctors aren’t trained to know when a brand is truly needed.Bottom Line
You shouldn’t automatically assume a brand-name drug is better. For most medications, the generic is just as safe and effective. But for a small group of drugs - those with narrow therapeutic windows, or where inactive ingredients cause problems - the brand matters. It’s not about money. It’s about precision. If your doctor prescribes a brand-name drug, don’t assume it’s unnecessary. Ask why. Be informed. Be proactive. Your health is worth the conversation.Can my pharmacist switch my brand-name drug to a generic without telling me?
In 49 U.S. states and Washington D.C., pharmacists can substitute a generic unless the doctor writes "do not substitute" or "brand medically necessary" on the prescription. In Texas, rules vary by drug class. If your prescription doesn’t say otherwise, your pharmacist can switch it - and they’re not always required to notify you. Always check your pill bottle and ask if the medication changed.
Are generic drugs less effective than brand-name drugs?
For most medications, no. A 2020 analysis of 47 studies with over 112,000 patients found no difference in outcomes between brand and generic versions of statins, blood pressure meds, and antidepressants. The FDA requires generics to be bioequivalent, meaning they deliver the same amount of active ingredient into your bloodstream. The exception is narrow therapeutic index drugs like levothyroxine, warfarin, and levetiracetam, where even small differences can matter.
Why do some people have side effects after switching to a generic?
Generics must contain the same active ingredient, but they can use different inactive ingredients - like fillers, dyes, or coatings. For most people, this doesn’t matter. But some individuals are sensitive to these additives. For example, one generic version of ciprofloxacin might contain lactose, causing stomach upset in someone with dairy sensitivity. If you notice new symptoms after switching, tell your doctor and pharmacist. You may need to go back to the brand or try a different generic.
How do I know if my drug is a narrow therapeutic index (NTI) drug?
Common NTI drugs include levothyroxine (Synthroid), warfarin (Coumadin), levetiracetam (Keppra), phenytoin (Dilantin), and lithium. You can check the FDA’s Orange Book online or ask your pharmacist. If your doctor prescribes one of these and says "do not substitute," it’s because switching could affect your treatment. Don’t assume it’s unnecessary - these drugs require precision.
What if my insurance won’t cover the brand-name drug?
If your doctor says you need the brand for medical reasons, they can file a prior authorization request. This is paperwork explaining why the generic won’t work. Approval rates vary - 89% for antiepileptics, but only 45% for acid reflux drugs. If denied, you can appeal. Some drug manufacturers offer patient assistance programs. You can also ask about authorized generics - made by the brand company but sold cheaper - which may be covered.






Aidan McCord-Amasis
November 15, 2025 AT 04:38Generics are fine unless you’re on Synthroid. Then it’s a nightmare. I switched and felt like a zombie for 3 months. Back to brand - instant life back. 💀
Katie Baker
November 16, 2025 AT 11:30Thank you for writing this. So many people don’t realize how much these tiny differences matter. I’ve been on warfarin for 10 years and my INR goes nuts if they switch me. My doctor fights for me every time. 🙏
Hollis Hollywood
November 17, 2025 AT 09:30I’ve been a pharmacist for 18 years and I can tell you - most of the time, generics are perfect. But I’ve seen too many patients come in with new seizures, fatigue, or panic attacks after a switch. It’s not about money. It’s about the fillers, the coating, the absorption curve. One guy told me he felt like his brain was underwater after switching from Keppra. He cried when he got his brand back. I don’t blame him. The FDA’s 80-125% range? That’s like saying your airplane can fly between 500 and 1,000 feet and it’s still safe. It’s not. For some meds, precision isn’t optional - it’s survival. I wish more doctors understood this before they just let the pharmacy swap. And I wish insurance companies would stop treating these like they’re interchangeable toothpaste.
Edward Ward
November 17, 2025 AT 12:21It’s fascinating, isn’t it?-how we’ve built a system that prioritizes cost-efficiency over biological individuality? The FDA’s bioequivalence standards were designed for mass production, not for human physiology. And yet, we treat every drug like it’s a bolt from Home Depot-interchangeable, standardized, disposable. But the human body? It’s not a machine. It’s a symphony of micro-variations. A 5% difference in absorption? For some, it’s a seizure. For others, it’s a depression spiral. For others, it’s nothing. And yet, we reduce it all to a checkbox on a form. We’re not just saving money-we’re gambling with people’s lives, and calling it ‘efficiency.’
Adam Dille
November 19, 2025 AT 03:12My mom switched from Synthroid to generic and started having heart palpitations. She thought it was stress. Turns out, her TSH went from 2.1 to 8.7. She didn’t even know it happened until her next blood test. Now she refuses to switch. And honestly? I get it. Why risk it? 😌
Jonathan Dobey
November 19, 2025 AT 10:39Let’s be real: the pharmaceutical industry doesn’t care about your health. They care about patents expiring. Generics are a corporate convenience. The FDA? A puppet. The whole system is rigged to push you toward the cheapest option-even if it kills you slowly. And the worst part? They don’t tell you. You wake up one day with a different pill, no warning, no consent. It’s medical gaslighting. And they call it ‘progress.’
Jessica Chambers
November 20, 2025 AT 13:29So… you’re saying if I take a generic blood pressure pill and suddenly start seeing ghosts, it’s the dye? Not my soul leaving my body? 😏
Chris Bryan
November 22, 2025 AT 01:36This is why America is failing. We let corporations dictate medicine. The government lets them. Doctors just sign the forms. And we wonder why people are sick. It’s not the pills. It’s the system. Stop pretending generics are ‘safe.’ They’re just cheaper. And cheaper means disposable. You’re not a patient-you’re a cost center.
Shyamal Spadoni
November 22, 2025 AT 14:40you know what this is really about? the fda is owned by big pharma. they let the generics in because they want you to get addicted to the brand then switch you to the cheap one so you dont notice. its all a scam. i know a guy in delhi who got seizures after switching his epilepsy med. he had to fly to germany to get the real one. the usa is a medical colony. they dont care if you die as long as the stock price goes up. #pharmacracy
Ogonna Igbo
November 23, 2025 AT 04:22Why are Americans so scared of generics? In Nigeria, we use generics for everything. Even for cancer. If you can’t afford the brand, you die. That’s life. You don’t cry because your pill looks different. You take it. Your body doesn’t care if it’s made in New Jersey or Lagos. This obsession with brand names is a luxury problem. We don’t have time for your placebo psychology.
BABA SABKA
November 23, 2025 AT 17:44Let’s cut the corporate BS. The real issue isn’t bioequivalence-it’s control. The brand-name companies want you dependent on their product. They lobby to keep NTI drugs off the generic list. They pay doctors to prescribe their names. And they bury the data when generics cause problems. Meanwhile, the FDA just rubber-stamps everything because they’re underfunded. It’s not about science. It’s about market dominance. And the patient? Just a revenue stream.
Andrew Eppich
November 25, 2025 AT 05:06It is regrettable that some individuals persist in attributing medical outcomes to trivial factors such as pill coatings. The scientific consensus is clear: bioequivalence, as defined by the FDA, is sufficient for therapeutic equivalence. To suggest otherwise is to undermine evidence-based medicine and promote unfounded fear. Patients should be educated to trust regulatory bodies, not anecdotal stories.
ASHISH TURAN
November 25, 2025 AT 19:47My dad’s on levothyroxine. He switched to generic, had a stroke. Not because of the drug-because the pharmacy gave him the wrong one. The bottle said Synthroid but it was a different generic. He didn’t check. I learned: always check the label. Even if it’s the same company, different batches can have different fillers. Always ask. Always verify. Don’t assume.
John Foster
November 27, 2025 AT 09:53There is a deeper metaphysical question here: if a pill performs identically in a lab but not in a body, does it truly exist as the same substance? The FDA measures blood concentration, but not consciousness. Not the tremor in the hand. Not the fog in the mind. Not the silence where laughter used to be. We quantify the chemical, but ignore the human. We have the data, but we’ve lost the meaning. The brand-name drug is not just a molecule-it is a ritual, a promise, a continuity of self. To replace it is not to substitute a chemical-it is to erase a memory. And memory, in medicine, is not optional. It is the foundation of trust. And trust, once broken, cannot be bioequivalent.