Black Box Warning Checker
Check Your Prescription Medication
Enter the name of your prescription medication to see if it has an FDA black box warning and learn what it means for you.
Enter a medication name to see if it has a black box warning.
When you pick up a prescription, you might notice a small, bold, black-bordered box on the medication insert. It looks like a warning label you’d see on a power tool or a ladder. But this isn’t about accidents-it’s about life-threatening risks. This is a black box warning, and it’s the strongest safety alert the FDA can require for a prescription drug.
Over 400 prescription medications in the U.S. carry this warning as of 2025. That’s about 15% of all prescription drugs on the market. You might be taking one right now and not even realize it. The warning doesn’t mean the drug is unsafe. It means the risks are serious enough that your doctor must pause, think, and talk to you before prescribing it.
What Exactly Is a Black Box Warning?
A black box warning, officially called a boxed warning by the FDA, is a mandatory safety notice printed in a thick black border on the prescribing information for a drug. It’s not optional. It’s not a suggestion. It’s the highest level of safety alert the agency can issue. These warnings appear after a drug has been on the market for years and real-world use reveals serious, sometimes deadly, side effects that weren’t caught in clinical trials.
Before a drug gets this warning, the FDA doesn’t just guess. They look at data from millions of patients. The MedWatch program, the FDA’s system for tracking adverse drug events, receives over 1.2 million reports every year. When patterns emerge-like a spike in heart attacks among users of a certain diabetes drug-the agency digs deeper. If the evidence shows a clear, preventable risk of death or permanent injury, they demand the warning be added.
There are four main reasons the FDA requires a black box warning:
- The drug causes serious side effects where the risks may outweigh the benefits for some patients.
- The side effects can be avoided if the drug is used in a specific way-like not giving it to pregnant women or avoiding alcohol while taking it.
- The drug is only approved for use in very limited situations, like treating a rare cancer or when other treatments have failed.
- The drug is especially dangerous for certain groups, such as children, the elderly, or people with specific health conditions.
Once a black box warning is added, it rarely disappears. The FDA requires overwhelming evidence to remove it. Since 2000, only 12 warnings have been fully lifted.
Why Do These Warnings Exist?
Drug trials are done on a few thousand people over months or a couple of years. But real life is messy. Millions of people take a drug for years. They have other health problems. They take other medications. They don’t follow instructions perfectly. That’s when hidden dangers show up.
Take rosiglitazone, a diabetes drug. After years on the market, studies showed it increased the risk of heart attacks. The FDA added a black box warning in 2007. Usage dropped by 70%. But even then, over 3 million people were still getting it because doctors and patients felt the benefits for some still outweighed the risks.
Another example is fluoxetine (Prozac). It carries a black box warning for increased suicidal thoughts in children and teens during the first few weeks of treatment. That doesn’t mean kids shouldn’t take it. It means doctors must monitor them closely in the beginning. For many, the drug is life-changing. For others, the risk is too high.
The warning isn’t there to scare you. It’s there to make sure you and your doctor make an informed choice. It’s a conversation starter.
What Does It Mean for You?
Here’s the thing most people get wrong: A black box warning doesn’t mean stop taking the drug. It means understand the risk before you take it.
A 2023 survey found that 78% of patients said they’d want to know if their medication had a black box warning. But only 42% remembered their doctor ever discussing it. That’s a huge gap. Many people find out from a Google search or a pharmacy label-and panic.
Pharmacists in Vancouver, Toronto, and Seattle report the same thing: patients show up with printed pages from the internet, scared, and ask, “Should I stop this?” The answer is almost always: “Don’t stop. Talk to your doctor.”
Some drugs with black box warnings are essential. clozapine, for example, is one of the most effective treatments for severe schizophrenia. But it can cause a life-threatening drop in white blood cells. So patients must get weekly blood tests. The warning makes sure no one skips that step.
Another example: valproate (Depakote). It’s used for epilepsy and bipolar disorder. But if a woman takes it while pregnant, it can cause severe birth defects. The warning says: “Do not use in women of childbearing potential unless other treatments fail.” It’s not a ban. It’s a rulebook for safe use.
How Doctors Use These Warnings
Doctors don’t just read the warning and move on. They have to actively consider it. The FDA requires that before prescribing any drug with a black box warning, the doctor must:
- Review the patient’s full medical history.
- Check for drug interactions.
- Assess whether the patient is in a high-risk group.
- Explain the risks clearly and confirm the patient understands.
- Consider alternatives.
Many doctors now use checklists or electronic alerts in their systems. If a patient has liver disease and the doctor tries to prescribe a drug with a black box warning for liver damage, the system flags it. That’s how these warnings work in practice: not as a stop sign, but as a red flag that says, “Slow down. Think.”
Some drugs with black box warnings are only given under special programs called Risk Evaluation and Mitigation Strategies (REMS). These programs require extra steps-like mandatory training for prescribers, regular lab tests, or even signing a form acknowledging the risk. You might not know you’re in a REMS program. Your pharmacist will tell you if you are.
What You Should Do If Your Medication Has a Black Box Warning
If you find out your medication has a black box warning, don’t panic. Don’t stop. Do this:
- Read the warning-not just the box, but the full explanation in the patient leaflet. It will tell you what the risk is and who it affects.
- Ask your doctor: “What’s the risk for me? Is it preventable? Are there safer options?”
- Ask your pharmacist: “Do I need special monitoring? Blood tests? Avoiding anything?”
- Don’t skip follow-ups. If your doctor says you need a blood test every 4 weeks, show up. Missing one could be dangerous.
- Don’t rely on online forums. Reddit, Facebook groups, and YouTube videos can be misleading. Stick to what your medical team says.
Some patients avoid taking a needed medication because of a black box warning. That’s often worse than the risk. A 2024 study in Cureus found that patients who stopped taking antidepressants with black box warnings due to fear had higher rates of hospitalization for depression than those who stayed on treatment with proper monitoring.

How the System Is Changing
The FDA is getting faster. In the past, it took 18 to 24 months to add a black box warning after a safety signal was found. Now, thanks to the Drug Safety Communications program and AI-powered monitoring tools, the average time is down to 6-9 months. In 2022 alone, the FDA added or updated 37 black box warnings.
By 2025, the FDA plans to roll out a new AI system that can scan millions of medical records and social media reports to spot danger signals faster. It’s not perfect, but it’s designed to catch risks before they become epidemics.
There’s also talk of “dynamic labeling”-digital warnings that update in real time as new data comes in. Imagine opening your pharmacy app and seeing a pop-up: “New data: This drug may increase stroke risk in patients over 75. Talk to your doctor.” That’s the future.
Final Thought: It’s Not About Fear. It’s About Awareness.
Black box warnings aren’t meant to keep you from getting better. They’re meant to help you get better safely. They exist because drugs are powerful. Sometimes, the same thing that heals can also harm. The warning doesn’t say, “Don’t take this.” It says, “Know what you’re getting into.”
If you’re on a medication with this warning, you’re not alone. Millions are. Many are thriving. The difference? They didn’t ignore it. They talked about it. They asked questions. And they stayed in control of their care.
Do black box warnings mean a drug is unsafe?
No. A black box warning means the drug has serious, potentially life-threatening side effects that require special caution. Many drugs with these warnings are still essential treatments. The warning ensures that doctors and patients weigh the risks and benefits before using the drug. For example, clozapine has a black box warning for blood disorders, but it’s often the only effective treatment for severe schizophrenia.
Can I stop taking my medication if it has a black box warning?
Never stop a prescription medication without talking to your doctor first. Stopping suddenly can cause serious withdrawal effects or make your condition worse. If you’re concerned about the warning, schedule a visit to discuss your options. Your doctor may adjust your dose, switch you to another drug, or add monitoring to keep you safe.
Why don’t I hear about black box warnings from my doctor?
Studies show that doctors often don’t discuss black box warnings during prescribing, even though they’re required to. This doesn’t mean they’re ignoring the risk-it may be that they assume you’ve read the leaflet or they’re pressed for time. If you’re unsure, ask: “Does this medication have any serious risks I should know about?” Most doctors will welcome the question.
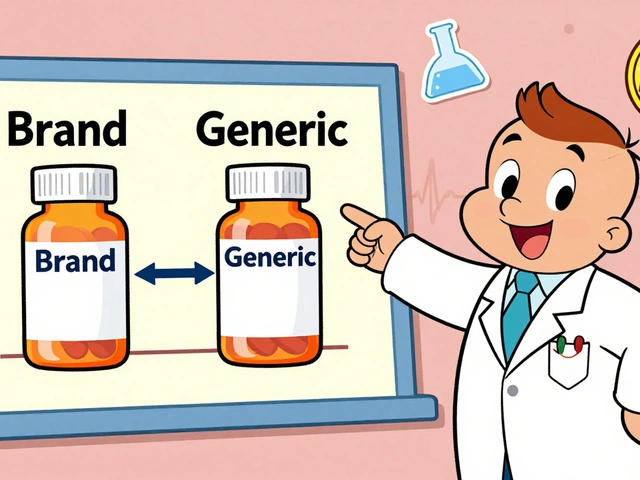
Are black box warnings only for brand-name drugs?
No. Both brand-name and generic drugs carry the same black box warnings because they contain the same active ingredient. For example, if the brand-name drug Prozac has a warning for increased suicidal thoughts in young adults, so does every generic version of fluoxetine. The warning is based on the drug’s chemistry, not the manufacturer.
Can a black box warning be removed?
Yes, but it’s rare. The FDA requires strong evidence that the original risk no longer exists or has been significantly reduced. Since 2000, only 12 black box warnings have been fully removed. Most stay because the underlying risk-like organ damage or birth defects-remains real even if the drug is used carefully.
Do other countries have black box warnings?
Other countries have similar systems, but they’re not called “black box warnings.” The European Medicines Agency (EMA) uses “contraindications” and “precautions” in drug summaries. Canada’s Health Canada uses “boxed warnings” too, though the format and frequency differ slightly. The U.S. system is the most visible and strictest in the world, with over 400 active warnings as of 2025.



Neha Motiwala
February 12, 2026 AT 12:16So let me get this straight-the FDA waits for people to die before they put a warning on a drug? That’s not safety, that’s a graveyard policy. I’ve seen people on clozapine, and yes, it works-but their white blood cells drop like a rock. Why not test every single person before prescribing? Why wait for a pattern in millions? They’re playing Russian roulette with our lives and calling it science.
Robert Petersen
February 14, 2026 AT 11:10Hey, I just want to say this article was super helpful. I was freaked out when I saw the black box on my antidepressant, but now I get it-it’s not a death sentence, it’s a heads-up. My doc explained everything, and I’m doing way better. Don’t panic, don’t quit. Talk. That’s the key.
Reggie McIntyre
February 15, 2026 AT 08:25Black box warnings are the pharmaceutical equivalent of a neon sign that says ‘DANGER: THIS THING CAN KILL YOU BUT ALSO SAVE YOU.’ It’s wild how we treat meds like candy until the FDA slaps a coffin on the label. I used to think these were just corporate scare tactics-until my aunt’s doctor caught her liver enzyme spike thanks to the warning on a common painkiller. Turns out, the system works… just barely.
Carla McKinney
February 15, 2026 AT 10:10Let’s be honest: most doctors don’t read these warnings either. They’re rushed, distracted, and still rely on outdated pamphlets. The FDA’s system is flawed if it depends on patients stumbling upon the warning online. And don’t get me started on pharmacists-half of them can’t pronounce the drugs they’re dispensing. This isn’t safety. It’s a broken feedback loop with extra steps.
Gloria Ricky
February 17, 2026 AT 07:44i just found out my zoloft has a black box warning and i was like… wait what? i’ve been on it for 5 years. my dr never mentioned it. i called them today and they said ‘oh yeah, we all know about it’-but never told me. kinda feels like they assume you’re dumb if you don’t google it. i’m not mad, just… confused? thanks for the article, it helped me ask better questions.
Stacie Willhite
February 18, 2026 AT 17:26I’ve been on valproate for 12 years. I’m a woman, I’m not pregnant, and I’ve never had a bad reaction. But I still get my blood drawn every month. I used to resent it-until I saw a friend who skipped hers and ended up in the ER. This warning? It’s not about fear. It’s about showing up. Even when you think you’re fine. Especially then.
Jason Pascoe
February 18, 2026 AT 22:54As someone from Australia, I find it fascinating how the U.S. system is so visible with these black boxes. Over here, we have warnings too-but they’re buried in fine print. No bold borders, no drama. Maybe that’s why people here panic more? The U.S. turns medical risk into a headline. Not sure if that’s better or worse… but it definitely gets attention.
Rob Turner
February 19, 2026 AT 17:18It’s funny how we treat drugs like they’re magic wands. You take one, boom-cured. But they’re more like dynamite. The black box isn’t a scare tactic-it’s a reminder that healing isn’t simple. That every pill has two sides: one that mends, one that breaks. And sometimes, the same hand that gives you hope… can take it away. We need more of this awareness, not less.
Gabriella Adams
February 20, 2026 AT 20:08Dynamic labeling is the future. Imagine your pharmacy app alerting you: ‘New data: This drug increases stroke risk in patients over 75.’ That’s not sci-fi-that’s the next step. We’re moving from static warnings to real-time risk assessment. The FDA’s AI system? It’s clunky, but it’s the first time we’ve tried to listen to the data, not just the headlines. Finally.
Annie Joyce
February 22, 2026 AT 05:27My grandma’s on clozapine. She’s 81, paranoid, and hasn’t slept in 3 years-until this drug. Now she’s smiling again. The black box says ‘blood tests every week.’ We do them. No big deal. But people online act like it’s a death sentence. It’s not. It’s just… a little more responsibility. And honestly? That’s okay.
Sophia Nelson
February 22, 2026 AT 14:18So the FDA waits for people to die, then slaps on a warning… and we’re supposed to be grateful? This isn’t safety-it’s damage control with a fancy label. They knew about the heart risks with rosiglitazone for years. Why wait? Because lawsuits cost more than warnings. This system is broken, and we’re all just playing along.