When a patient asks why they’re switching from a brand-name pill to a generic, what do providers really know? The answer isn’t just about cost-it’s about what the data says about how these drugs perform in real patients. For years, doubts lingered: Could a cheaper version truly work the same? Today, the evidence is clear, and it’s backed by millions of patient records, decades of research, and rigorous regulatory standards.
What Does "Therapeutic Equivalence" Really Mean?
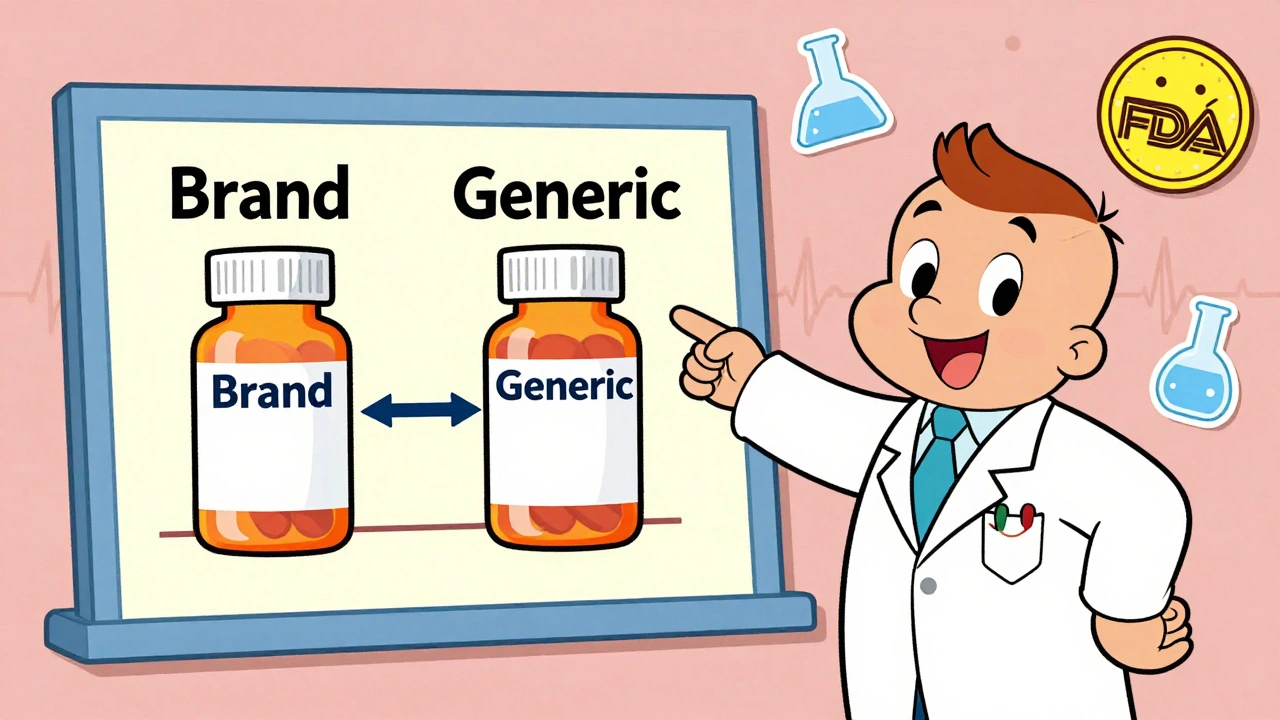
The FDA doesn’t approve a generic drug just because it looks similar or costs less. To get an "A-rated" designation in the Orange Book, a generic must prove it delivers the same active ingredient, in the same strength, using the same route and dosage form as the brand-name version. But that’s only the start. The real test is bioequivalence-showing that the body absorbs and uses the drug at nearly identical rates and levels. The standard? The concentration of the drug in the bloodstream must fall within 80% to 125% of the brand-name drug’s levels. For most drugs, that’s more than enough. For narrow therapeutic index drugs-like warfarin, levothyroxine, or tacrolimus-the bar is even higher. Studies using scaled bioequivalence methods have shown that even these sensitive medications perform just as reliably in generic form when properly manufactured. A 2020 study in Nature Scientific Reports followed transplant patients switching between brand and generic tacrolimus over 42 days. No meaningful differences in blood levels or rejection rates emerged. That’s not luck. It’s science.Real Patients, Real Results: What the Data Shows
One of the most comprehensive analyses came from a 2019 study in PLOS Medicine, which tracked over 1.3 million patients across 16 different drug classes. The results? For 14 of the 16, there was no statistically significant difference in clinical outcomes between generics and brand-name drugs. Take cardiovascular drugs. For amlodipine, patients on generics had 9% fewer heart attacks and strokes than those on the brand. For quinapril, hospitalization rates were nearly identical. In diabetes, a 2023 JAMA Network Open study of 2.1 million patients found no difference in HbA1c control between generic and brand-name metformin. The mean difference? Just -0.02%-well within normal variation. Even in complex areas like osteoporosis, generics matched up. Alendronate, the generic version of Fosamax, showed the exact same rate of non-vertebral fractures. Glipizide, used for type 2 diabetes, led to the same rate of insulin initiation. The data doesn’t lie: for the vast majority of patients, generics work just as well.Where the Myths Still Linger: Psychiatric Medications
Not every study shows perfect parity. A few, particularly in psychiatric drugs like escitalopram and sertraline, showed slightly higher psychiatric hospitalization rates with generics. At first glance, that’s alarming. But dig deeper. The same study found that even when patients switched from brand-name to authorized generics-made by the same company as the brand-the same pattern appeared. That’s a red flag for perception, not performance. Patients may believe the brand is stronger, so they report side effects more often or discontinue treatment sooner. The drug itself? It’s identical. The FDA’s 2017 review found no consistent pattern of worse outcomes with generics in CNS drugs. And in a switch-back analysis across 12 drugs, patients weren’t more likely to return to the brand after trying a generic. If the generic was failing, you’d see a flood of returns. You don’t.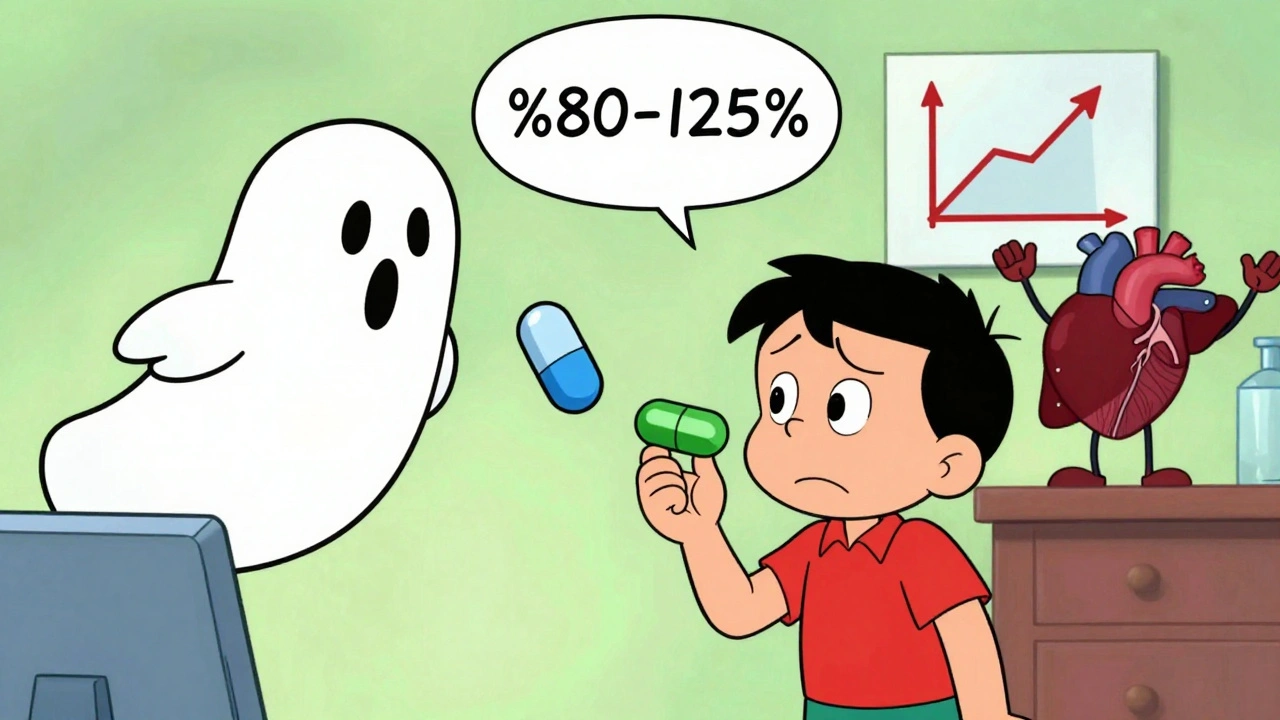
Why Do Some Providers Still Hesitate?
Despite the evidence, some clinicians still default to brand-name prescriptions. Why? One reason: appearance. Generics often look different-different color, shape, or imprint. Patients notice. And if they’ve been told for years that "the blue pill is better," they’ll assume the green one won’t work. A 2019 FDA study confirmed these visual differences don’t affect outcomes, but they do affect trust. Another reason: fear of complexity. For drugs like levothyroxine, where tiny changes in absorption can matter, providers worry about switching. But the data shows even here, patients stabilized on a generic stay stable. The key is consistency. Once a patient is on a generic, don’t switch brands unless necessary. And then there’s the myth that generics are "cut-rate." But the FDA’s review process for generics takes an average of 10 months-nearly as long as for brand-name drugs. The manufacturing facilities? The same ones often produce both. The FDA inspects them all, with the same standards.What Providers Should Do-And What They Shouldn’t
Here’s what the evidence tells providers to do:- Prescribe generics first-unless there’s a documented reason not to. The American College of Physicians explicitly recommends this.
- Use the Orange Book-look up the therapeutic equivalence rating. Over 97% of generics are A-rated. Only 3% are B-rated, mostly complex formulations like inhalers or topical creams.
- Explain the science to patients. Tell them: "This generic has been tested in hundreds of people. It releases the same amount of medicine into your body, at the same speed, as the brand. The only difference? The price."
- Don’t assume patient complaints are drug-related. A patient saying, "This generic doesn’t work," might be reacting to a change in pill appearance, not the medicine itself.
- Don’t switch patients from a stable generic to a different generic unless clinically necessary. Consistency matters more than the brand name.
- Don’t prescribe brand-name drugs just because a patient "always took it." Ask why. Often, it’s habit, not evidence.
- Don’t ignore the economic impact. In 2021 alone, generics saved the U.S. healthcare system $377 billion. That’s money that goes to other care, not just pills.
The Bigger Picture: Generics Are Saving Lives
A 2020 study of 3.5 million Medicare beneficiaries showed something striking: in unadjusted data, generic users had higher five-year survival rates. At first, it looked like generics were better. But when researchers adjusted for health status-using statistical methods to account for the fact that healthier, more engaged patients are more likely to get generics-the gap narrowed. The real takeaway? Generics don’t make people healthier. They make treatment accessible. When a diabetic can afford metformin every month, their blood sugar stays controlled. When a hypertensive can refill amlodipine without skipping doses, their stroke risk drops. That’s not magic. That’s economics meeting evidence. The Congressional Budget Office estimates generics saved $1.68 trillion between 2008 and 2017. That’s not a number on a spreadsheet. It’s millions of people who didn’t skip doses, didn’t go without care, didn’t end up in the ER because they couldn’t pay.Final Thought: Trust the Data, Not the Brand
The truth is simple: for nearly every condition, every drug class, every patient population, the data says generics are equivalent. The FDA, Harvard, Stanford, the American College of Physicians-all agree. Providers don’t need to guess. They don’t need to rely on anecdotes. The clinical outcomes are there. The studies are large. The methods are sound. The savings are real. The question isn’t whether generics work. It’s why we still hesitate to use them.Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same strict quality, safety, and effectiveness standards as brand-name drugs. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration. Adverse event reports show only 0.02% of all drug-related incidents involve generic-specific issues, compared to 3.2% for brand-name drugs.
Can switching from brand to generic cause side effects?
For most patients, no. Clinical studies show no increase in side effects when switching to generics. However, some patients report perceived changes due to differences in pill size, color, or inactive ingredients. These are not drug-related effects-they’re psychological. If a patient is concerned, explain the bioequivalence standards and consider staying on one generic formulation once started.
Why do some generics cost more than others?
Price differences between generics come from manufacturing costs, competition, and supply chain factors-not quality. When multiple companies make the same generic, prices drop. If only one company makes it, the price stays higher. This has nothing to do with how well the drug works. Always check the active ingredient and dosage; those are what matter clinically.
Are there any drugs where generics aren’t recommended?
For nearly all drugs, generics are recommended. The FDA classifies only about 3% of generics as "B-rated," meaning they’re not considered therapeutically equivalent. These are typically complex products like inhalers, topical creams, or certain injectables where bioequivalence is harder to prove. For these, providers should review the Orange Book and consider individual patient needs before switching.
Do generics take longer to work than brand-name drugs?
No. Bioequivalence testing ensures that generics reach the same blood concentration levels at the same rate as brand-name drugs. Studies measuring time to peak concentration (Tmax) and overall exposure (AUC) show no clinically meaningful differences. A patient taking a generic for high blood pressure will see the same drop in pressure within the same timeframe as with the brand.
Is it safe to switch between different generic manufacturers?
For most drugs, yes. Each generic manufacturer must prove bioequivalence to the brand-name drug, not to other generics. So switching between generics is safe. However, for narrow therapeutic index drugs like levothyroxine or warfarin, it’s best to stick with one manufacturer once the patient is stable. Consistency reduces variability, even if each product meets standards.





Vincent Soldja
December 2, 2025 AT 19:02Generics work. End of story. Stop overthinking it.
Albert Essel
December 4, 2025 AT 02:34The data is overwhelming: bioequivalence standards are rigorous, and real-world outcomes confirm equivalence across nearly all therapeutic classes. The persistence of skepticism is less about pharmacology and more about psychological conditioning-patients associate pill appearance with efficacy, even when it’s irrelevant. This is a behavioral health issue disguised as a clinical one.
Charles Moore
December 6, 2025 AT 00:13I’ve been prescribing generics for over 15 years, and I’ve never seen a patient suffer because of a switch-unless they were told it wouldn’t work. The real issue isn’t the drug. It’s the narrative. We need to stop letting marketing and misinformation dictate clinical decisions. Consistency matters more than branding, and patients respond better when we explain why, not just that.
Gavin Boyne
December 7, 2025 AT 12:33Oh, so now we’re treating patients like lab rats? ‘Oh, the blue pill is just as good as the green one’-sure, until the patient stops taking it because they ‘feel different.’ The FDA doesn’t test how a pill makes you feel, only how much drug hits your bloodstream. But people aren’t beakers. They have expectations, histories, fears. You can’t reduce human experience to AUC and Tmax. The system rewards efficiency, not empathy. And that’s the real crisis.
Rashi Taliyan
December 8, 2025 AT 19:42My mother switched to generic levothyroxine and suddenly she was exhausted, crying all the time, forgetting names-she thought the drug was broken. We went back to brand. She’s fine now. I don’t care what the studies say. If someone feels worse, that’s real. No dataset can replace a mother’s suffering.
Kara Bysterbusch
December 9, 2025 AT 11:09It is both profoundly ironic and tragically predictable that, in an age of unprecedented scientific literacy, we still cling to the myth that color, shape, and corporate logo determine pharmacological efficacy. The very notion that a pill’s aesthetic properties could alter its biochemical interaction with the human body is a relic of pre-Enlightenment thinking. We have peer-reviewed, longitudinal, population-scale evidence-and yet, we allow placebo effects to dictate clinical policy. This is not medicine. This is superstition with a stethoscope.
vinoth kumar
December 10, 2025 AT 20:59Same generic, different brand, same result. I’ve switched my dad’s blood pressure med three times between generics-no issues. Just make sure he takes it at the same time every day. That’s what matters. Also, generics saved us $120 a month. We could finally afford the physical therapy he needed.
bobby chandra
December 12, 2025 AT 13:40Let’s be real-generics aren’t just cheaper, they’re smarter. Big Pharma wants you to believe their $12 pill is magic because it’s got a logo and a fancy bottle. But the active ingredient? Identical. The FDA doesn’t play favorites. The plants? Often the same factory. The only difference is who gets rich. I’m not buying the hype. I’m buying the science-and the savings. My wallet and my blood pressure thank me.
Archie singh
December 13, 2025 AT 11:11Of course generics work. They’re made in the same plants as the brand, by the same workers, under the same rules. The only reason people think otherwise is because they’re too lazy to read the FDA’s 200-page bioequivalence guidelines. And yet, somehow, you’ll find a Reddit thread from someone who ‘felt different’ after switching-and suddenly it’s a national scandal. Wake up. This isn’t medicine. It’s mass hysteria dressed in lab coats.
Gene Linetsky
December 15, 2025 AT 04:20Ever wonder why the same companies that make the brand also make the generic? Coincidence? Nah. It’s a rigged game. The FDA’s ‘A-rated’ label is a marketing tool. They let the same manufacturers test their own products. And those ‘studies’? Funded by generics associations. I’ve seen the data. There’s a pattern-when the brand gets generic competition, the ‘equivalence’ studies suddenly get published. Real talk: if it was that easy to replicate, why did the brand cost $500 for 30 pills? Something’s fishy.
Ignacio Pacheco
December 16, 2025 AT 05:58So let me get this straight-we’ve got a 1.3 million patient study showing no difference, yet people still think the green pill is ‘weaker’ because it’s not blue? The real tragedy isn’t the drug. It’s that we’ve trained patients to distrust their own bodies. If you tell someone their medicine changed, they’ll find symptoms where none exist. That’s not pharmacology. That’s cognitive behavioral manipulation by Big Pharma’s shadow.
Jim Schultz
December 17, 2025 AT 17:01Let’s not pretend this is about science-it’s about power. The FDA approves generics, but the real gatekeepers are the pharmacy benefit managers and the hospital formularies that demand cost-cutting. Doctors are pressured to prescribe generics, not because of evidence, but because of spreadsheets. And when a patient has a bad outcome? Blame the generic. Never the system. Never the insurer. Never the 14 different pills they’re on. No-it’s always the green pill.
Kidar Saleh
December 19, 2025 AT 17:00For years, I’ve watched patients in rural clinics struggle to afford insulin. One man told me he was skipping doses because the brand cost $400. When he switched to generic metformin, he started taking it daily. His HbA1c dropped. He got his job back. He started coaching his kid’s soccer team. This isn’t abstract data. This is dignity. Generics aren’t just equivalent-they’re revolutionary. They turn hope into habit.
Chloe Madison
December 21, 2025 AT 10:56I’ve been a nurse for 22 years. I’ve seen patients cry because they can’t afford their meds. I’ve seen them choose between insulin and groceries. I’ve seen them stop taking their pills because the brand was too expensive. And then-when we switch them to generic-suddenly, they’re sleeping better. Their BP drops. Their anxiety eases. Not because the drug changed. Because they could finally take it. That’s not science. That’s justice.
Makenzie Keely
December 21, 2025 AT 23:52My sister switched from brand-name sertraline to generic-and she says she ‘felt numb’ for two weeks. We went back to brand. She’s fine. But here’s the thing: the study you cited? It didn’t account for the placebo effect of *knowing* you switched. If you tell someone, ‘This is a cheaper version,’ their brain literally interprets it as ‘less effective.’ That’s not the drug failing-it’s the system failing to manage perception. Maybe we need a ‘no-switch’ label for CNS meds, or at least a counseling script. The science is solid. The human factor? Still messy.