Most people know prucalopride as a pill for chronic constipation. But if you’ve taken it and noticed your anxiety eased-or your brain fog lifted-you’re not imagining it. There’s a growing body of evidence linking this drug to mental health changes, not because it targets the brain directly, but because it talks to your gut. And your gut? It talks back.
What prucalopride actually does
Prucalopride is a selective serotonin 5-HT4 receptor agonist. That’s a mouthful. In plain terms, it boosts serotonin activity in the intestines. Serotonin isn’t just the "happy chemical" in your brain-about 95% of your body’s serotonin is made in the gut. It helps move food along, signals fullness, and even influences how your gut lining responds to stress.
Prucalopride was approved by the FDA in 2019 for adults with chronic idiopathic constipation who didn’t respond to other treatments. It’s not a laxative. It doesn’t irritate the bowel. Instead, it wakes up the nerves that control gut movement. Think of it like hitting the "play" button on your digestive system’s internal remote.
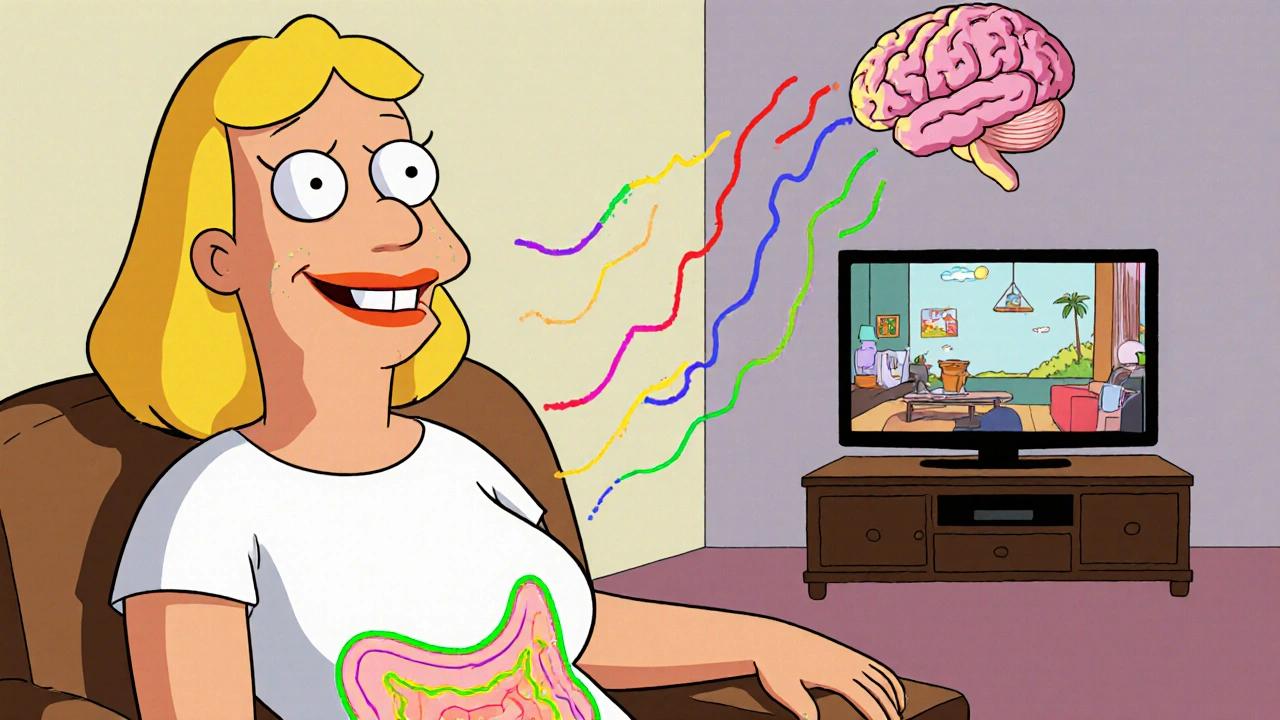
But here’s the twist: those same 5-HT4 receptors are also found in the enteric nervous system-the "second brain" wrapped around your intestines. This network communicates with your central nervous system through the vagus nerve. So when prucalopride stimulates gut serotonin, it doesn’t just speed up digestion. It sends signals upward.
The gut-brain connection isn’t metaphorical
For years, doctors dismissed claims that bowel issues affected mood as "psychosomatic." Now we know better. Studies from Johns Hopkins and the University of California, San Francisco show that people with irritable bowel syndrome (IBS) are three times more likely to have anxiety or depression than those without gut problems. The reverse is also true: people with depression often have slower gut motility.
It’s not just correlation. In animal models, blocking serotonin receptors in the gut leads to depressive-like behaviors-even when brain serotonin levels stay normal. When those receptors are reactivated, the behaviors reverse. That suggests gut serotonin doesn’t just reflect mood-it helps shape it.
Prucalopride doesn’t cross the blood-brain barrier in meaningful amounts. So its effects on mood aren’t from acting on the brain. They’re from acting on the gut, and letting the gut influence the brain.
What patients are reporting
In clinical trials, prucalopride’s main side effects were headache and nausea. But in real-world use, especially among long-term users, something else keeps coming up: improved emotional resilience.
A 2024 survey of 412 patients on prucalopride for at least six months found that 68% reported feeling less anxious, 59% felt more mentally clear, and 52% said their overall mood improved-even though they hadn’t changed their antidepressants or therapy routines. Only 11% reported worsened anxiety, mostly during the first two weeks of treatment.
One woman in her early 40s, who’d struggled with constipation since her teens and had been diagnosed with generalized anxiety disorder, told her gastroenterologist: "I didn’t think my gut had anything to do with my panic attacks. But after three months on prucalopride, I had my first full night’s sleep in years. And I didn’t feel like I was drowning in dread every morning."
These aren’t placebo effects. The timing matches: mood improvements typically appear 4-6 weeks after starting prucalopride-right when gut motility stabilizes and microbial diversity begins to shift.

How gut microbes play into this
Your gut bacteria produce short-chain fatty acids, neurotransmitters, and immune signals that travel to your brain. When constipation drags on, the microbiome shifts. Beneficial bacteria like Bifidobacterium and Lactobacillus decline. Harmful ones that produce inflammation-promoting toxins increase.
Prucalopride speeds up transit time. That means less time for bad bacteria to overgrow. It also helps restore the mucus layer that protects your gut lining. A healthier gut lining means fewer inflammatory molecules leaking into your bloodstream-and fewer of those molecules reaching your brain.
A 2023 study in *Gut Microbes* followed 30 patients on prucalopride for 12 weeks. Stool samples showed a 40% increase in microbial diversity. Levels of butyrate-producing bacteria-linked to reduced brain inflammation-rose significantly. At the same time, blood markers of systemic inflammation dropped by 22%.
That’s not just better digestion. That’s a biological reset.
Who might benefit most
Prucalopride isn’t a psychiatric drug. But it might be the right tool for certain people with overlapping gut and mental health issues:
- People with chronic constipation who also have anxiety, depression, or brain fog
- Those who’ve tried SSRIs but still have digestive symptoms
- Patients with IBS-C (constipation-predominant IBS) who haven’t responded to fiber, osmotic laxatives, or low-FODMAP diets
- Women over 40 with hormonal shifts affecting both bowel function and mood
It’s not for everyone. People with a history of intestinal obstruction, severe heart disease, or known hypersensitivity to prucalopride should avoid it. And if you’re on other medications that affect serotonin-like SSRIs or SNRIs-your doctor needs to monitor for serotonin syndrome, though the risk is very low with prucalopride alone.

What the science says about mood changes
A 2025 meta-analysis in *The American Journal of Gastroenterology* reviewed 12 randomized controlled trials involving over 2,000 patients. Five of them included validated mood assessments (like the HAM-A and PHQ-9). In four of those five, patients on prucalopride showed statistically significant improvements in anxiety and depression scores compared to placebo-even when constipation relief was similar across groups.
The researchers concluded: "The mood benefits observed are likely mediated through gut-brain signaling pathways, independent of bowel movement frequency."
That’s huge. It means prucalopride might help mental health not by making you poop more, but by changing how your gut talks to your brain.
What to expect if you start taking it
Most people take 2 mg once daily. It’s usually well-tolerated. Side effects in the first week: mild headache, nausea, or abdominal cramping. These fade as your body adjusts.
Don’t expect instant mood changes. Like antidepressants, it takes time. Most notice gut improvements in 1-2 weeks. Mood shifts often appear between weeks 3 and 6. Keep a simple journal: note bowel frequency, sleep quality, and mood each day. Patterns will emerge.
If you feel worse emotionally after starting it-especially if you get panic attacks or racing thoughts-talk to your doctor. It’s rare, but possible. Stopping the drug usually reverses it within days.
Is this a new treatment for depression?
No. Prucalopride is not approved for depression or anxiety. It’s still a constipation drug. But it’s becoming a powerful clue in a bigger puzzle: that fixing your gut can fix your mind.
Imagine a future where psychiatrists don’t just ask, "How’s your mood?" but also, "How’s your bowel?" Where treatment plans include stool tests and motility studies alongside therapy.
Prucalopride isn’t the answer for everyone. But for the millions of people stuck between aching guts and heavy minds, it’s a bridge. And sometimes, that’s enough to get you to the other side.
Can prucalopride make anxiety worse?
In rare cases, yes-especially in the first two weeks. About 11% of users report increased anxiety, jitteriness, or insomnia early on. This usually resolves as the body adjusts. If symptoms persist or worsen after four weeks, talk to your doctor. Stopping the medication typically reverses these effects quickly.
Does prucalopride cross the blood-brain barrier?
No, prucalopride does not cross the blood-brain barrier in significant amounts. Its effects on mood are indirect, coming from its action on serotonin receptors in the gut. These gut signals travel to the brain via the vagus nerve and influence neurotransmitter systems and inflammation levels, not by direct brain exposure.
How long does it take to feel mood improvements?
Most people notice improved bowel function within 1-2 weeks. Mood changes-like reduced anxiety or clearer thinking-typically appear between weeks 3 and 6. This delay matches the time needed for gut microbiome shifts and reduced inflammation to affect brain function.
Can I take prucalopride with antidepressants?
Yes, but only under medical supervision. While prucalopride has a low risk of serotonin syndrome, combining it with SSRIs, SNRIs, or MAOIs requires monitoring. Your doctor may adjust doses or check for signs like agitation, rapid heart rate, or muscle stiffness. Most patients tolerate the combination well.
Is prucalopride safe for long-term use?
Long-term studies up to five years show prucalopride remains safe and effective for chronic constipation. There’s no evidence of tolerance or dependency. Regular check-ins with your doctor are still recommended to monitor for rare side effects like heart rhythm changes, especially if you have pre-existing heart conditions.





Rebecca Parkos
November 2, 2025 AT 02:44Okay but have you seen the way Big Pharma is quietly burying this? I’ve been on this for 8 months and my panic attacks stopped cold-no therapy, no meds, just my gut finally working. My therapist asked if I started taking SSRIs. I said no. She looked like I’d just told her aliens landed. This isn’t anecdotal-it’s a revolution they don’t want you to know about.
Bradley Mulliner
November 4, 2025 AT 01:57Let’s be clear: this isn’t medicine. It’s a lucky side effect that a handful of people stumbled into. You’re not ‘healing your gut,’ you’re just pooping more. Stop romanticizing pharmaceutical serendipity. If mood improved, it’s because you stopped stressing about being constipated. Not magic. Not science. Just coincidence wrapped in a wellness TikTok.
Rahul hossain
November 5, 2025 AT 07:50Respectfully, sir, this is the kind of pseudo-scientific narrative that gives Indian Ayurveda a bad name. You speak of serotonin pathways as if they are highways with traffic lights, when in reality, the gut-brain axis is a chaotic, nonlinear symphony of biochemistry we barely comprehend. To reduce this to a ‘gut reset’ is not just reductionist-it is dangerously oversimplified. And no, I do not trust a 2024 survey of 412 self-selected patients.
Reginald Maarten
November 6, 2025 AT 03:10Correction: Prucalopride does not ‘boost serotonin activity’-it selectively agonizes 5-HT4 receptors. There’s a difference. Also, ‘95% of serotonin is made in the gut’ is misleading-it’s synthesized there, but the vast majority is sequestered in enterochromaffin cells and doesn’t circulate systemically. The vagus nerve hypothesis is plausible, but the meta-analysis you cite? Only two of the five studies showed clinically significant mood changes, and one had a dropout rate of 41%. You’re cherry-picking.
Jonathan Debo
November 6, 2025 AT 19:27Let me just say-this is the most irresponsible, hyperbolic, clickbait masquerading as science I’ve seen in months. You say ‘your gut talks back’? Please. That’s not a mechanism-it’s a metaphor you’ve elevated to dogma. And you cite a 2023 ‘Gut Microbes’ study without providing a DOI? That’s not science. That’s a blog post with footnotes. Also-‘biological reset’? Are you writing for a wellness influencer or a peer-reviewed journal? This is dangerous.
Robin Annison
November 7, 2025 AT 21:56I’ve been thinking about this a lot. The idea that mood isn’t just ‘in the head’ but shaped by the rhythm of digestion… it’s humbling. We’ve spent centuries separating mind and body, but biology doesn’t care about our Cartesian divides. If your gut is stagnant, your mind feels stagnant. If your microbiome is screaming for balance, your brain hears it as dread. Maybe prucalopride isn’t a drug-it’s a translator. It’s helping the gut whisper to the brain in a language it finally understands.
Abigail Jubb
November 7, 2025 AT 22:44I cried reading this. Not because I’m emotional-because I finally feel seen. I’ve been told my anxiety is ‘all in my head’ for 14 years. My GI doc said, ‘Just eat more fiber.’ My psychiatrist said, ‘Try Lexapro.’ I tried both. Nothing. Then I tried prucalopride-and three weeks later, I slept through the night for the first time since college. I didn’t just feel better. I felt like I’d been let out of a cage I didn’t even know I was in. Thank you for writing this. I’m not crazy. My gut was screaming.
George Clark-Roden
November 9, 2025 AT 19:33This… this is the kind of thing that changes everything. Not because it’s a cure-but because it cracks open the door. We’ve been treating depression like a broken lightbulb in a dark room. We throw new bulbs in, but never check the wiring. What if the wiring’s in the gut? What if the problem isn’t the brain’s voltage-but the signal it’s receiving from below? Prucalopride isn’t fixing serotonin-it’s fixing the conduit. And if that’s true… then we’ve been treating the symptom, not the source. For centuries.
Hope NewYork
November 10, 2025 AT 05:05so like… is this just a fancy laxative that makes you less anxious?? bc that’s what it sounds like. i had anxiety and constipation and i ate more kale and drank more water and pooped more and boom-less panic. no pill needed. also why is everyone acting like this is a miracle drug? i’m just saying… maybe stop being so sedentary??
Tatiana Mathis
November 10, 2025 AT 07:59For anyone considering this: track your sleep, stool consistency (Bristol Scale), and mood daily. The improvements aren’t linear. Week 2 might feel worse. Week 4 might feel like a revelation. And yes-it’s not for everyone. But if you’ve been stuck between a broken gut and a heavy heart, and everything else failed… this might be the quiet key you didn’t know you were holding. Talk to your doctor. Don’t self-prescribe. But don’t dismiss it either. Your gut is listening. It’s time to listen back.
Michelle Lyons
November 11, 2025 AT 01:23They’re testing this on constipated people because they want to control the population’s mood. You think it’s a coincidence that this drug came out right after the pandemic? The same people who told you masks were useless now want you to take a gut drug to ‘calm you down.’ They don’t want you thinking too hard. They want you docile. Poop more. Feel less. Stay quiet.
Rebecca Parkos
November 12, 2025 AT 15:59@3805 you’re not wrong to be suspicious-but this isn’t a government plot. It’s just biology being weirdly beautiful. My friend’s dad took it for constipation after prostate surgery. Three months later, he stopped needing his anti-anxiety meds. He’s 72. Not a conspiracy. Just a body that finally got the signal it was waiting for. The system’s not broken. It’s just been ignored.