When a pharmacist hands you a pill that looks different from what you’ve been taking for years, it’s natural to feel uneasy. That’s even more true when it’s your child’s medicine or your own. Generic drugs are just as safe and effective as brand-name ones - but communication makes all the difference. Too often, patients are told, "It’s the same thing," and left with unanswered questions. For kids and older adults, that simple phrase isn’t enough. It can even backfire.
Why Generic Substitution Feels Risky to Parents and Seniors
Parents worry because their child’s medicine isn’t just a pill - it’s a routine, a ritual, sometimes the only thing standing between their child and a hospital visit. Brand-name pediatric medications often come in sweet-tasting liquids, chewable tablets, or easy-to-swallow capsules. Generics? Many don’t. A 2019 FDA analysis found only 32% of generic pediatric formulations match the taste or form of the brand. One parent on Reddit shared: "My 2-year-old refused the generic amoxicillin because it tasted like bitter soap. We switched back, even though it cost $40 more." For seniors, the issue is different. Many take four or more medications daily. When a blood pressure pill changes color, shape, or size - again - they stop taking it. A 78-year-old woman in a 2023 AARP forum said: "My pill changed three times in six months. I thought I was getting a different drug. I stopped until my doctor explained each one." That’s not confusion - it’s a safety risk.The Science Behind Generic Drugs (And Why It’s Not Enough)
The FDA requires generics to have the same active ingredient, strength, and route of delivery as the brand. They must also be bioequivalent - meaning they absorb into the body within 80% to 125% of the brand’s rate. That sounds precise. But here’s the catch: for drugs with a narrow therapeutic index - like seizure medications, thyroid pills, or blood thinners - even small differences in absorption can matter. A 2017 Danish study followed nine patients switched from brand to generic epilepsy drugs. Four had seizure relapses. Their labs showed no change in dosage - just a change in the pill. And for kids? The FDA admits: "Without pediatric studies before a drug goes generic, it’s very unlikely to ever get them." That means many generics for children are just adult pills crushed or split - not tested for safety or taste in little bodies. For seniors, metabolism slows. Liver and kidney function change. A dose that’s perfect for a 50-year-old might be too strong for an 80-year-old. But generic labels rarely reflect that.What Works: Communication That Builds Trust
Saying "It’s the same" doesn’t work. Patients hear: "It’s cheaper. It’s not as good." That’s the nocebo effect - when expecting harm causes real symptoms. A 2021 study in Frontiers in Pharmacology found 58% of seniors reported new side effects after switching to a generic - even when no clinical change occurred. The fix? Three steps:- Explain the science simply. "This pill has the same medicine inside as your old one. It’s made by a different company, so it looks different, but it works the same way. The FDA checks it to make sure."
- Use the teach-back method. Ask: "Can you tell me in your own words why we’re switching?" If they say, "So I don’t have to pay so much," that’s good. If they say, "So it’s weaker," you’ve got work to do.
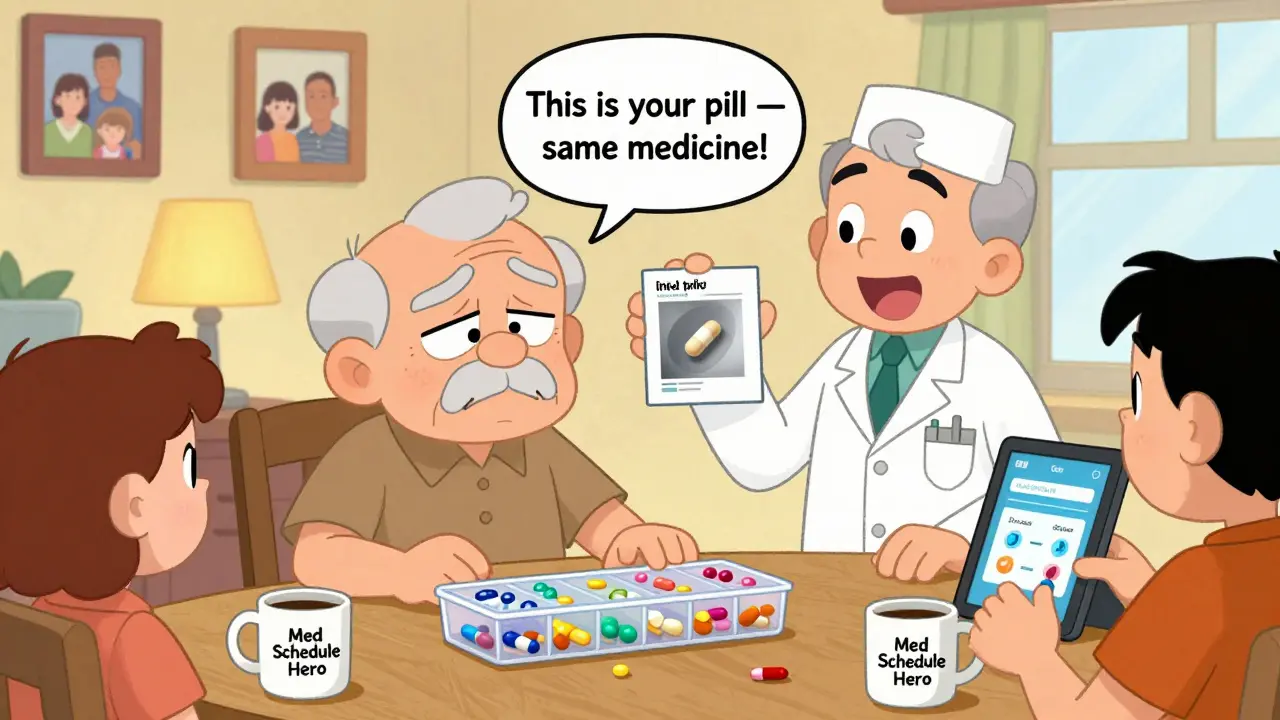
- Address the physical change. Show them the old and new pill side by side. Say: "This is your old pill. This is the new one. Same medicine. Different shape. Same dose. We’re not changing how much you take."
Special Rules for Pediatric Patients
For children, communication starts with parents. Don’t assume they know generics are safe. A 2020 Pediatrics study found 62% of parents are hesitant. They’re not irrational - they’ve seen their child refuse a bitter-tasting generic and get sick because they didn’t take their full dose. Pharmacists should:- Ask: "Has your child ever had trouble taking this medicine before?"
- Offer alternatives: "We have a generic with a fruit flavor. Or we can order the brand if cost is a concern."
- Never substitute without checking the formulation. A liquid generic for a 6-month-old with reflux might be crushed tablets mixed with water - not the same as the original suspension designed for infants.
Special Rules for Senior Patients
Seniors need more than words - they need structure. Many have memory issues, poor eyesight, or trouble reading small print. A 2022 study in the Journal of the American Pharmacists Association showed that using the teach-back method improved adherence by 32% in seniors. Here’s how to help:- Use large-print labels. Write the drug name in bold, 14-point font.
- Include a photo of the pill on the label. Many seniors recognize pills by sight, not name.
- Involve a family caregiver. Don’t just hand the prescription to the patient. Say: "I’d like to walk through this with your daughter too."
- Initiate the conversation before the switch. Don’t wait until they notice the pill changed. Call ahead: "Your blood pressure pill is switching to a new version next month. We’ll send you a picture and a note so you know what to expect."
What to Avoid
Don’t say:- "It’s just as good." (Too vague. Sounds dismissive.)
- "The insurance won’t cover the brand." (Makes them feel pressured.)
- "Everyone takes generics." (Invalidates their concern.)
- "I understand this change might feel strange. Let’s talk about why we’re doing it and what to watch for."
- "Your child’s medicine is being changed because the new version is cheaper, but it’s the same active ingredient. We’ll check in next week to make sure it’s working."
- "If you feel different after the switch, call us right away. We’ll help you figure out why."

What’s Changing in 2026
New FDA guidelines released in June 2023 require generic manufacturers to include clear information about formulation differences in patient materials - especially for kids and seniors. Some states are now considering laws to stop automatic substitution for high-risk drugs like epilepsy or heart medications in these groups. And digital tools are helping: apps that let seniors take a photo of their pill and get instant identification are now used by 67% of seniors who switched to generics - and they report feeling more confident.When to Stick With the Brand
Cost matters. But so does safety. If a child refuses a generic because of taste - and it leads to missed doses - the brand may be worth the extra cost. If a senior has had three different generic versions of the same pill in a year and keeps mixing them up - the brand might be the safer choice. Talk to your doctor. Ask: "Is this switch medically necessary, or just financially convenient?"Final Thought: It’s Not About the Pill. It’s About the Person.
A pill is just a pill. But for a parent, it’s peace of mind. For a senior, it’s independence. Generic substitution saves the U.S. healthcare system $373 billion a year. But if patients stop taking their medicine because they don’t understand the change, those savings vanish - replaced by ER visits, hospitalizations, and lost trust. The best generic substitution isn’t the cheapest one. It’s the one the patient understands - and believes in.Are generic drugs really as effective as brand-name drugs?
Yes, for most people and most medications, generics are just as effective. The FDA requires them to contain the same active ingredient, strength, and dosage form as the brand. They must also be bioequivalent - meaning they work in the body at nearly the same rate and amount. But for drugs with a narrow therapeutic index - like epilepsy, thyroid, or blood thinner medications - even small differences in absorption can matter. That’s why communication and monitoring are critical, especially for children and older adults.
Why do generic pills look different from brand-name ones?
By law, generic drugs can’t look exactly like the brand-name version - that would violate trademark rules. So they use different colors, shapes, or markings. But the medicine inside is the same. The difference is only in the inactive ingredients - things like dyes, fillers, or coatings. These don’t affect how the drug works, but they can affect taste, how easy it is to swallow, or whether a child will refuse it.
Can I ask my pharmacist to give me the brand-name drug instead?
Yes. In most cases, you can request the brand-name drug even if a generic is available. Your pharmacist may need to check with your doctor or insurance, but they can usually fill the prescription as written. If cost is a concern, ask if there’s a patient assistance program, coupon, or mail-order option that makes the brand more affordable. Your health and ability to take the medicine consistently matter more than saving a few dollars.
What should I do if my child refuses to take the generic medicine?
Don’t force it. If your child refuses the generic because of taste or texture, contact your pharmacist or doctor. Ask if there’s a flavored version, a different formulation (like a chewable), or if the brand is available at a lower cost through a savings program. Missing doses because of refusal can be more dangerous than paying more for the original medicine. Your child’s health isn’t a trade-off.
My senior parent keeps mixing up their pills after switching to generics. What can we do?
Start by using a pill organizer with clear labels and large print. Ask your pharmacist to include a photo of each pill on the prescription label. Consider using a medication identification app - many seniors find them helpful. Most importantly, involve a family member in medication reviews. Schedule a monthly check-in to go over each pill: name, purpose, and appearance. If substitutions happen often, ask the doctor if switching to a brand-name version for key medications would reduce confusion and improve safety.
Is it safe to switch between different generic brands of the same drug?
Technically, yes - all generics must meet FDA standards. But switching between different generic versions can cause problems, especially for seniors or children. Each version may have slightly different inactive ingredients, which can affect how the drug is absorbed. If someone has been stable on one generic, switching to another can trigger side effects or reduced effectiveness. Ask your doctor or pharmacist to stick with one generic manufacturer if possible. If a switch happens unexpectedly, monitor closely and report any changes.




Erwin Kodiat
January 18, 2026 AT 17:03Man, I never thought about how much stress these pill changes cause for seniors. My grandma stopped taking her blood pressure med for two weeks because the color changed. She thought she was getting scammed. We had to sit down with her and show her the old vs new side by side. Now she takes pics of every new pill with her phone. It’s wild how something so small can break trust.
Also, why do pharmacies never tell you in advance? It’s like a surprise attack.
Jacob Hill
January 20, 2026 AT 06:57This is spot-on. I’m a pharmacist, and I’ve seen the same thing over and over. Parents think the generic is ‘watered down’ because it’s not sweet. Seniors think the new pill is a different drug because it’s blue instead of white. We’re not just dispensing medicine-we’re managing fear.
The teach-back method? It’s not optional anymore. If they can’t explain it back, we haven’t done our job. And yes, sometimes the brand is worth the cost. No shame in that.
Malikah Rajap
January 22, 2026 AT 00:10Ohhh, I love this so much!! I mean, really-how is it that we live in a world where a pill’s color can trigger a full-blown existential crisis in an 80-year-old?? And yet, we treat it like it’s just a logistics issue??
It’s not about chemistry, it’s about identity. The pill is a ritual. A symbol. A tiny anchor in a world that’s slipping away. When it changes, they don’t just feel confused-they feel abandoned. And that’s not just medical-it’s spiritual. We need to stop treating patients like data points and start treating them like people who’ve lived through wars, heartbreaks, and birthdays. The pill? It’s just the container. The meaning? That’s the medicine.
Astha Jain
January 23, 2026 AT 19:04generic? lol. in india we just get the same pill with a different label and 10x cheaper. no one cares. why is america so dramatic? also, my cousin’s kid took generic amoxicillin and cried for 3 hours. we just mixed it with jam. problem solved. why make it so hard?
Jake Rudin
January 24, 2026 AT 06:58There’s a deeper metaphysical question here: If a pill performs identically but looks different, is it the same object? Or is identity tied to form? The FDA says yes, but the human mind says no. We don’t just consume chemicals-we consume narratives. The brand-name pill carries the narrative of safety, of corporate trust, of ‘this is what doctors use.’ The generic? It carries the narrative of compromise. And narratives, my friends, are more powerful than bioequivalence percentages.
That’s why the placebo effect works. And why the nocebo effect kills.
Phil Hillson
January 25, 2026 AT 06:31THIS IS WHY AMERICA IS BROKE. PEOPLE ARE TOO LAZY TO SWALLOW A PILLS. WHO CARES IF IT TASTES LIKE SOAP? MY GRANDPA TOOK HIS MEDS IN A BOWL OF CEREAL AND NEVER COMPLAINED. YOU WANT TO MAKE IT EASY? THEN DON’T HAVE KIDS OR BE OLD. SIMPLE.
Also, why are we letting pharmacists make medical decisions? Insurance companies should be the ones deciding what you get. End the nonsense.
Josh Kenna
January 26, 2026 AT 23:45As someone who’s watched my mom go through 5 different generic versions of her thyroid med in 2 years-I’m furious. One time she got a pill that made her heart race. We called the pharmacy, they said ‘oh, that’s just a different manufacturer.’ NO. THAT’S NOT ACCEPTABLE. I demanded she stay on the same generic brand. They charged me $80 extra. Worth every penny. My mom’s not a lab rat.
And yeah, the photo labels? YES. My mom doesn’t read. She recognizes faces. The pill’s face matters.
Valerie DeLoach
January 28, 2026 AT 23:06Thank you for writing this. I’ve been a nurse for 22 years, and I’ve seen too many elderly patients stop meds because they didn’t understand the switch. We need to train pharmacists like we train teachers. Not just ‘here’s your prescription,’ but ‘let’s sit down, look at the pill, and talk about how this works for YOU.’
Also-why aren’t we using pill identification apps as standard practice? They’re free, easy, and used by 67% of seniors who’ve switched. That’s not a tech trend-that’s a lifeline. Let’s make them mandatory on every prescription label.
And for parents? Don’t just say ‘it’s the same.’ Say ‘this one might taste bitter, so let’s try it with applesauce. If it doesn’t work, we’ll call your doctor. You’re not alone.’
Lydia H.
January 29, 2026 AT 01:22I’m a mom of a 4-year-old with asthma. We switched to a generic inhaler spacer and my kid started crying every time we used it. It smelled weird. Like plastic and sadness. We went back to the brand. $50 more a month. Worth it. I don’t care about the savings if my kid can’t breathe.
Also-why do we assume all parents are financially responsible? Some of us are just trying to survive. We don’t have time to research every pill. We need the system to work for us-not the other way around.
Christi Steinbeck
January 29, 2026 AT 06:18Y’all need to stop acting like this is a new problem. It’s been going on for decades. The solution? Empower patients. Give them the tools. Make them part of the team. Use apps. Use photos. Use teach-back. Use family. Use patience.
And if your insurance won’t cover the brand? Fight them. Call your doctor. Ask for a prior auth. Write a letter. Your health isn’t a spreadsheet. You’re not a cost center. You’re a human being who deserves to feel safe taking your medicine. Period.
And yes-sometimes the brand is worth it. Stop shaming people for choosing safety over savings.
Lewis Yeaple
January 30, 2026 AT 18:01It is imperative to note that the FDA’s bioequivalence criteria, while statistically valid, are not clinically infallible. The 80–125% confidence interval, derived from healthy adult populations, is fundamentally misaligned with pediatric and geriatric pharmacokinetics. This is not a communication failure-it is a systemic pharmacological oversight.
Furthermore, the absence of pediatric-specific bioequivalence studies constitutes a regulatory lacuna of considerable magnitude. The current paradigm is not merely inadequate-it is ethically indefensible.
sujit paul
January 31, 2026 AT 07:16Do you know who profits from generics? Big Pharma. They own the generics too. The same companies that sell you the brand-name drug. They just make you pay for the expensive version, then switch you to the cheap one-and still make money. It’s all a game. They don’t care if you live or die. They care about the stock price.
And the FDA? They’re just the cleaning crew for the casino. You think they’re protecting you? They’re protecting the system. Wake up.
Aman Kumar
February 1, 2026 AT 14:34The entire generic substitution paradigm is a neoliberal construct designed to externalize healthcare risk onto vulnerable populations. The linguistic framing of ‘it’s the same’ is a performative act of epistemic violence-erasing patient epistemology in favor of corporate hegemony. The pharmacokinetic variance, particularly in narrow-therapeutic-index drugs, is not an anomaly-it is a feature.
Moreover, the commodification of medical identity through pill aesthetics constitutes a semiotic rupture in the patient-provider relationship. We are not treating patients-we are managing compliance within a market-driven bio-political apparatus.
Tracy Howard
February 2, 2026 AT 16:34Canada doesn’t have this problem. We have universal healthcare and real drug regulation. Americans act like they’re surprised their system is broken. Of course it is. You let corporations run medicine. You think a pill should be a ‘brand’? That’s not medicine-that’s cereal.
Also, why are we even having this conversation? In Canada, we just give the cheapest one that works. If it doesn’t work, we switch. No drama. No fear. No ‘teach-back.’ Just medicine. Maybe America should try that.
Jackson Doughart
February 4, 2026 AT 06:59Thank you for this thoughtful, meticulously researched piece. The emphasis on communication-not just information-is profoundly correct. Trust is not built by regulatory compliance; it is built by presence, by listening, by honoring the emotional weight of routine and familiarity.
For pediatric patients, the caregiver’s anxiety is a clinical factor. For seniors, the pill’s appearance is a cognitive anchor. To dismiss either is to misunderstand the very nature of adherence.
What’s needed now is not more guidelines, but more time-time for pharmacists to sit, to show, to listen. And for that, we need systemic investment-not just in drugs, but in the human beings who dispense them.