Polypharmacy Risk Checker
Medication Risk Assessment
This tool estimates your risk of polypharmacy based on your current medication count and age. Polypharmacy (taking multiple medications) is common in older adults and can increase risk of side effects, falls, and hospitalizations. The goal isn't to stop all medications, but to ensure each one is truly beneficial.
Every year, millions of older adults take more medications than they need. Some of these drugs were prescribed years ago for conditions that have changed-or even disappeared. Yet they keep taking them, often because no one ever asked if they still needed them. This isn’t laziness or neglect. It’s a system that rewards adding pills, not removing them. The result? Higher risk of dizziness, falls, confusion, kidney damage, and hospital stays-all linked to medication side effects. The good news? There’s a proven way to fix this: deprescribing.
What Deprescribing Really Means
Deprescribing isn’t just stopping pills. It’s not a quick fix or a shortcut. It’s a careful, step-by-step process where doctors and patients work together to identify which medications might be doing more harm than good. The goal? Reduce unnecessary drugs without risking health. This approach is especially important for people over 65, who on average take five or more medications daily. That’s called polypharmacy-and it’s a silent crisis. According to the World Health Organization, about 40% of older adults globally are on potentially inappropriate medications. The idea took shape around 2010, led by researchers in Canada like Barbara Farrell and Cara Tannenbaum. They didn’t just say, “Stop the drugs.” They built tools-frameworks-that guide clinicians through the decision-making process. Today, deprescribing.org is the go-to resource for evidence-based protocols. These aren’t guesses. They’re based on clinical trials, expert reviews, and real patient outcomes.Which Medications Are Most Often Reduced?
Not all drugs are equal when it comes to deprescribing. Some have clear, well-studied risks. Five classes stand out as top targets:- Proton-pump inhibitors (PPIs) like omeprazole: Often prescribed for heartburn, but many people take them for years without a clear reason. Long-term use raises risk of bone fractures, kidney disease, and infections.
- Benzodiazepines and sleep aids like lorazepam or zolpidem: These can cause drowsiness, memory problems, and increase fall risk. Studies show many older adults can safely taper off these drugs over weeks.
- Antipsychotics used for behavioral issues in dementia: These are often prescribed off-label and carry a black-box warning for increased death risk in elderly patients with dementia.
- Antihyperglycemics like sulfonylureas: In older adults with limited life expectancy, aggressive blood sugar control can lead to dangerous low blood sugar episodes.
- Opioid painkillers: Many are prescribed long-term for chronic pain, even when benefits fade and risks climb. Tapering reduces addiction risk and improves alertness.
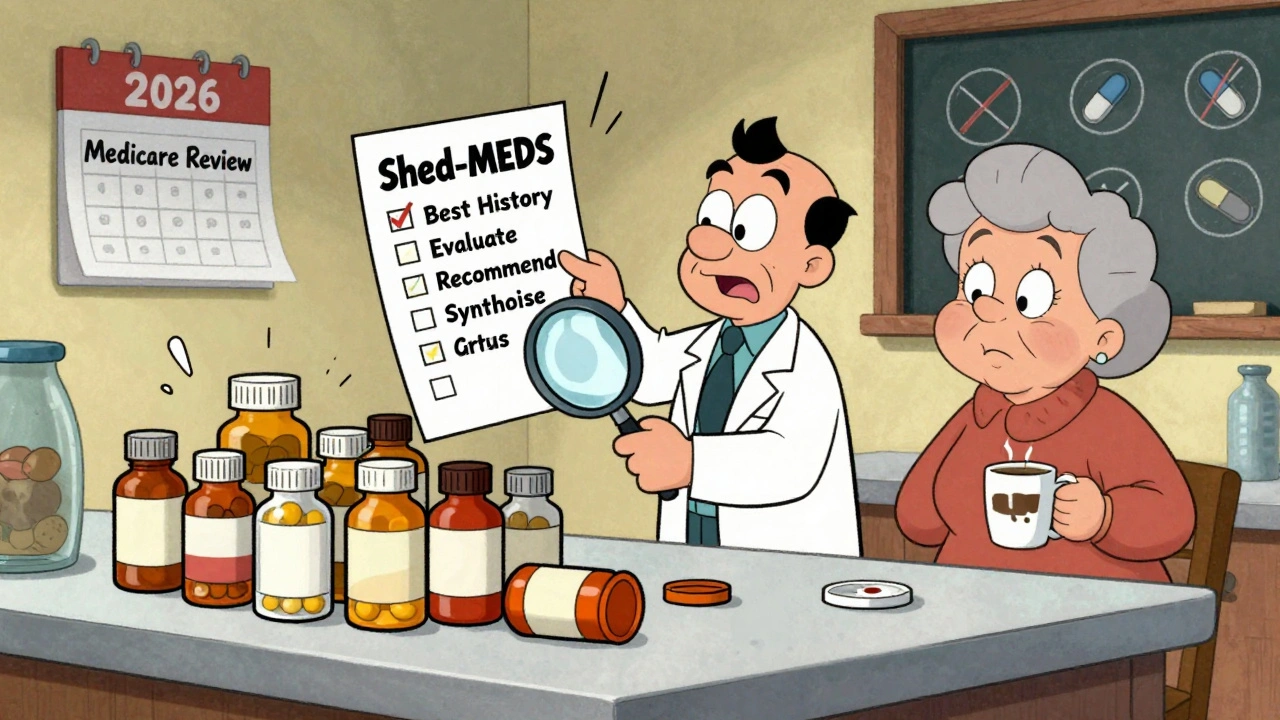
How It Works: The Shed-MEDS Framework
One of the most validated approaches is called Shed-MEDS. It stands for:- Best Possible Medication History-gather every drug the patient is taking, including over-the-counter and supplements.
- Evaluate-use tools like STOPP/START criteria or the Beers Criteria to flag potentially inappropriate meds.
- Deprescribing Recommendations-prioritize which drugs to cut first based on risk, benefit, and patient goals.
- Synthesis-create a clear plan with the patient, including tapering schedule and follow-up.
Why It’s Hard to Do-And How to Make It Work
You’d think this would be easy. But it’s not. Most doctors have 7-10 minutes per visit. Asking, “Which of these 12 pills can we take away?” takes time. It requires trust. It means having hard conversations. Patients often feel anxious. One woman in a 2022 study said, “I’ve been taking this pill for 20 years. What if I get sick without it?” That fear is real. And it’s why patient education is part of every good deprescribing plan. Nurses and pharmacists play a huge role here. In settings where pharmacists lead the process, success rates jump 35-40%. Electronic health records (EHRs) can help-but most don’t. Some systems now include alerts that say, “This patient is on a benzodiazepine. Consider deprescribing.” But only 32% of clinicians say their EHR actually supports this work. The rest are left to do it manually, with paper lists and memory. Successful programs require more than good intent. They need:- Pharmacists trained in medication therapy management (150+ hours of specialized training)
- Physician champions who model the behavior
- Nurses who monitor for withdrawal symptoms
- Time built into schedules-not squeezed in between other tasks
The Numbers Don’t Lie
Let’s talk about what this saves-not just in pills, but in money and lives. A 2023 Canadian study found that for every dollar spent on deprescribing programs, healthcare systems saved $3.20. How? Fewer hospital visits. Fewer emergency trips. Fewer falls. Fewer drug interactions. And it’s not just older adults. People with dementia, heart failure, or advanced cancer often get medications that don’t match their goals. A 2022 editorial in JAMA Internal Medicine warned that indiscriminate deprescribing can backfire-if done without understanding what matters to the patient. For someone with late-stage dementia, a pill that reduces agitation might improve quality of life, even if it doesn’t cure anything. Deprescribing isn’t about removing all drugs. It’s about removing the wrong ones. The American Geriatrics Society’s 2023 Beers Criteria lists 34 potentially inappropriate medications for seniors. But only 12 of them have formal deprescribing guidelines. That’s a big gap. Researchers are now working on protocols for antidepressants, anticoagulants, and other common drugs. By 2030, experts predict deprescribing checks will be as routine as checking blood pressure.
What You Can Do
If you or a loved one is on five or more medications, ask:- “Is this still needed?”
- “What happens if we stop it?”
- “Is there a safer alternative?”
- “Can we try reducing the dose slowly?”





Ernie Blevins
December 7, 2025 AT 13:27Ted Rosenwasser
December 9, 2025 AT 07:00Helen Maples
December 11, 2025 AT 05:37Ashley Farmer
December 12, 2025 AT 16:26David Brooks
December 13, 2025 AT 01:53Nicholas Heer
December 14, 2025 AT 03:17Sam Mathew Cheriyan
December 14, 2025 AT 04:08Nancy Carlsen
December 14, 2025 AT 04:18Jennifer Anderson
December 15, 2025 AT 01:53Sadie Nastor
December 15, 2025 AT 15:22Sangram Lavte
December 16, 2025 AT 09:41