It’s easy to assume that if you’re taking medications as prescribed, you’re safe. But what happens when two drugs you’re taking start working against each other? Or when your blood pressure drops suddenly after adding a new supplement? Drug interactions don’t always come with warning labels you can see. Sometimes, the first sign is your body screaming for help.
What Counts as a Dangerous Drug Interaction?
A drug interaction happens when one substance changes how another works in your body. This could be a prescription pill, an over-the-counter painkiller, a vitamin, an herbal remedy, or even grapefruit juice. The effects aren’t always obvious. One drug might make another stronger - so strong it becomes toxic. Or it might block it completely, leaving you unprotected against infection or a blood clot. The most dangerous interactions involve drugs with a narrow therapeutic index - meaning the difference between a helpful dose and a harmful one is tiny. Warfarin, digoxin, and phenytoin fall into this category. A 20% change in blood levels can mean the difference between control and crisis. That’s why people on these drugs need to be extra careful, especially when starting something new. Most serious interactions fall into three categories: drug-drug (about 60%), drug-food (20%), and drug-disease (20%). For example, if you have kidney disease and take NSAIDs like ibuprofen, you’re increasing your risk of kidney damage. Or if you’re on an antibiotic and eat grapefruit, you could end up with dangerously high levels of the drug in your blood.Symptoms That Require Emergency Care Right Now
Some reactions don’t wait. If you’re experiencing any of these, call 911 or go to the nearest emergency room immediately. Don’t wait to see if it gets better.- Difficulty breathing or oxygen levels below 90% - this can signal anaphylaxis, a life-threatening allergic reaction.
- Swelling of the face, lips, tongue, or throat - this can block your airway in minutes.
- Systolic blood pressure below 90 mmHg with a heart rate over 120 - your body is going into shock.
- Seizures lasting more than 2 minutes or sudden loss of consciousness - this could mean drug toxicity like lidocaine overdose.
- Body temperature above 41.1°C (106°F), rigid muscles, and extreme agitation - classic signs of serotonin syndrome, often triggered by mixing antidepressants with painkillers or cold medicines.
- High fever over 40°C (104°F), dark urine, and rapid heartbeat - possible neuroleptic malignant syndrome, a rare but deadly reaction to antipsychotics.
Symptoms That Need a Doctor Within 24 Hours
Not every reaction is an emergency. But some still need quick attention before they turn into one.- A widespread rash covering more than 30% of your skin - especially if it’s red, blistering, or peeling. This could be DRESS syndrome, a severe delayed reaction that can damage your liver or kidneys.
- Unexplained fever over 38.5°C (101.3°F) lasting more than two days - particularly if you’re on antibiotics or seizure meds. This might be serum sickness or another immune reaction.
- Unusual bruising or bleeding - if your platelet count drops below 100,000/μL, you’re at risk of internal bleeding. This can happen with certain antibiotics or blood thinners.
- Yellow skin or eyes, dark urine, or abdominal pain - these point to liver damage. ALT levels over 120 U/L are a red flag.
- Little or no urine output for six hours, plus rising creatinine - signs of drug-induced kidney injury, which accounts for nearly a quarter of all acute kidney failure cases in hospitals.
What Doctors Look For: The Clues They Use
Emergency physicians use specific patterns to spot serious interactions. One widely accepted rule from the American College of Emergency Physicians says: if you have two or more of these symptoms together, you’re likely having serotonin syndrome:- Heart rate over 100 bpm
- Fast breathing (more than 20 breaths per minute)
- Excessive sweating
- Dilated pupils
- Overactive reflexes
- Tremors
Real People, Real Mistakes
A 68-year-old woman in Vancouver started taking a new antidepressant and then picked up an over-the-counter cough syrup with dextromethorphan. She didn’t think twice - both were "safe." Within three days, she had tremors, sweating, and confusion. Her husband took her to the ER. She spent three days in intensive care. Her story isn’t rare. Reddit threads and patient forums are full of similar cases. One user on r/Pharmacy described getting fentanyl during a dental procedure while on an SSRI. Within minutes, he had clonus (involuntary muscle spasms), extreme sweating, and a racing heart. He ended up in the ICU. Meanwhile, a 2022 survey found that 58% of people waited more than 12 hours to call their doctor after noticing dizziness, nausea, or fatigue - symptoms they dismissed as "just tired." But those symptoms can be early warnings. The American Association of Poison Control Centers found that people who called poison control within an hour of noticing symptoms were 89% more likely to avoid the ER entirely.
How to Prevent This From Happening
The best way to avoid a dangerous interaction is to know what you’re taking - and tell your doctor everything.- Keep a current list of all medications, including vitamins, supplements, and herbal products. Don’t forget things like St. John’s Wort, turmeric, or garlic pills - they interact with blood thinners and antidepressants.
- Use a drug interaction checker like Drugs.com or Lexicomp. These tools screen over 24,000 medications and 500,000+ interactions. But you have to enter everything - including what you take occasionally.
- Ask your pharmacist to review your full list every time you pick up a new prescription. Pharmacists are trained to catch interactions doctors might miss.
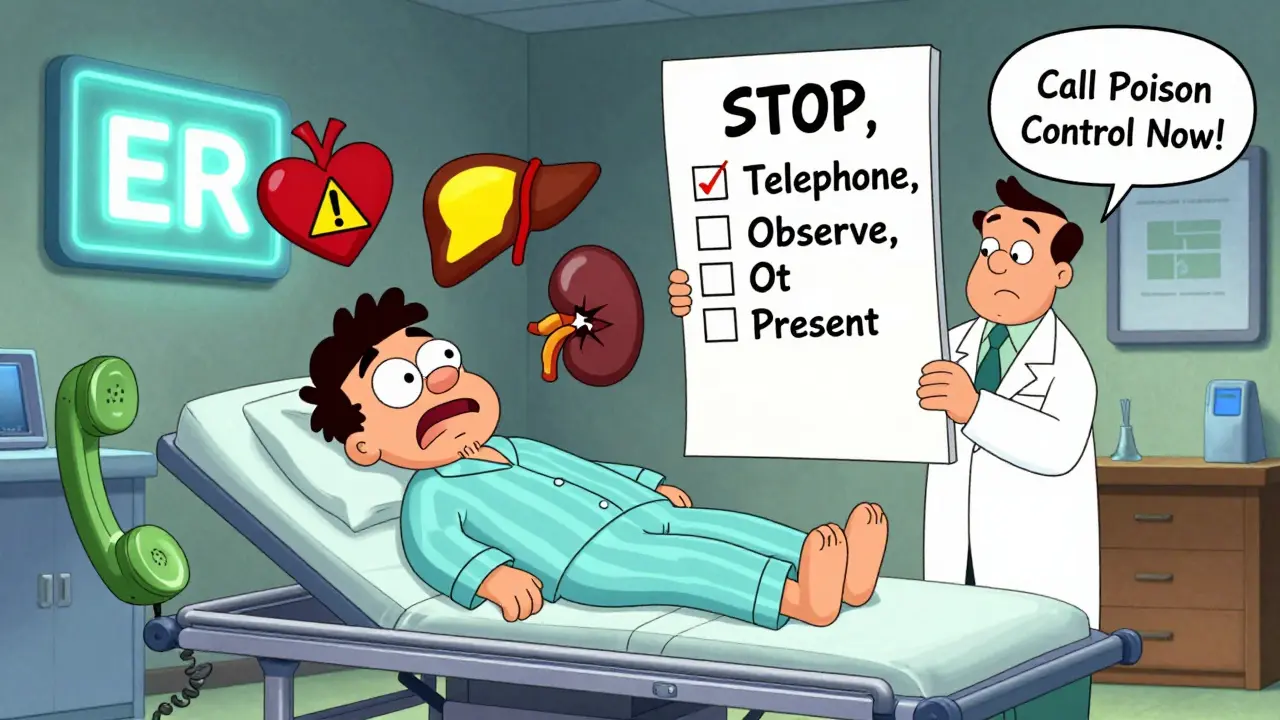
- Use the STOP protocol if you suspect a reaction: Stop taking the suspected drug, Telephone your provider, Observe your symptoms, and Present all your medication containers at your appointment.
Why This Matters More Than Ever
The average person over 65 takes five or more medications. At that point, your risk of a major interaction jumps to 57%. With 5.4 billion prescriptions filled each year in the U.S. alone, the chances of overlap are high. Even with electronic health records that are supposed to warn doctors about interactions, only 63% of systems properly grade the severity of those warnings. Many providers ignore alerts because they get too many - a problem called "alert fatigue." That’s why your awareness matters. No algorithm can replace your own body’s signals. If something feels off - if you suddenly feel dizzy, nauseous, weak, or confused - don’t assume it’s just stress or aging. It could be your drugs talking to each other in a way they shouldn’t.What to Do If You’re Unsure
If you’re not sure whether your symptoms are serious, call poison control. In Canada, it’s 1-844-POISON-1 (1-844-764-7661). They’re staffed 24/7 by pharmacists and nurses who know exactly what to ask. Most cases - 65% - are handled over the phone without needing a hospital visit. You don’t need to wait until your next appointment. You don’t need to Google symptoms until your anxiety spikes. If you’re on multiple drugs and something feels wrong, trust your gut. Call your doctor. Call poison control. Get help.Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC meds like ibuprofen, acetaminophen, antihistamines, and cough syrups can interact with prescription drugs. For example, mixing ibuprofen with blood thinners increases bleeding risk. Dextromethorphan in cough syrup can trigger serotonin syndrome when taken with SSRIs. Even supplements like St. John’s Wort can reduce the effectiveness of birth control pills or antidepressants.
What should I bring to the doctor if I suspect a drug interaction?
Bring all your medications - pills, patches, liquids, and supplements - in their original containers. This helps your doctor see the exact names, doses, and frequencies. Also bring a written list of what you take and when. Many people forget about herbal teas, CBD oil, or vitamins they only take once a week.
Can drug interactions happen even if I’ve taken the same meds for years?
Absolutely. Your body changes over time. Kidney or liver function slows with age. New conditions like thyroid disease or diabetes can alter how drugs are processed. Even a new supplement or dietary change - like starting a high-fiber diet or drinking more grapefruit juice - can trigger an interaction you never had before.
Are herbal supplements safe because they’re "natural"?
No. "Natural" doesn’t mean safe. St. John’s Wort can make birth control, antidepressants, and heart meds less effective. Garlic and ginkgo can thin your blood. Kava can damage your liver. Herbal supplements aren’t regulated like drugs, so their strength and ingredients can vary. Always tell your doctor what you’re taking - even if you think it’s harmless.
How can I check for interactions myself?
Use trusted tools like Drugs.com, Medscape’s Drug Interaction Checker, or your pharmacy’s app. Enter every medication, including vitamins and supplements. Don’t skip anything - even a daily multivitamin. These tools flag interactions based on current medical data and are updated regularly. But remember: they’re tools, not replacements for professional advice.
What if I can’t afford to stop a medication?
Never stop a prescribed medication without talking to your doctor first. But do tell them you’re worried about side effects. They may be able to switch you to a safer alternative, adjust the dose, or monitor you more closely. Many clinics have medication assistance programs. Pharmacists can also help you find lower-cost options or generic versions.
If you’re taking multiple medications, you’re not alone - but you shouldn’t have to guess whether you’re safe. Your health isn’t a risk you should manage alone. Ask questions. Speak up. And when in doubt, get help sooner rather than later.





Art Van Gelder
December 23, 2025 AT 07:21Man, I had no idea grapefruit juice could turn your meds into a time bomb. My grandpa swears by it for his cholesterol, never thought it might be killing him slowly. Now I’m scanning every label like a spy. And don’t even get me started on that dextromethorphan + SSRI combo - I’ve seen people post about feeling ‘weird’ after cough syrup and just brush it off. But serotonin syndrome? That’s not ‘weird,’ that’s your brain screaming in a language only ER doctors understand.
It’s wild how we treat our bodies like cars you just throw gas into and hope for the best. We don’t skip oil changes for our vehicles, but we’ll toss three new supplements in because ‘it’s natural.’
Kathryn Weymouth
December 24, 2025 AT 15:13Thank you for this comprehensive breakdown. The distinction between emergency symptoms and those requiring 24-hour attention is critical - too many people wait until they’re collapsing before acting. The CIOMS scale and STOP protocol are practical tools that should be printed on every prescription bottle. Also, the statistic about 65% of poison control cases being resolved without ER visits is a powerful reminder that help is just a phone call away. Don’t panic, but don’t ignore it either.
Herman Rousseau
December 25, 2025 AT 04:04Big shoutout to pharmacists - they’re the unsung heroes of medication safety. 🙌 I used to think they just handed out pills, but after my mom’s interaction scare with warfarin and turmeric, I started asking them to review everything. They caught a dangerous combo my doctor missed. Always bring your bottles. Always ask. You’re not bothering them - you’re saving your life.
And yes, ‘natural’ doesn’t mean ‘safe.’ Kava nearly took out my yoga instructor. We all need to stop romanticizing herbal stuff. 🌿💀
Johnnie R. Bailey
December 25, 2025 AT 10:35It’s funny how we trust algorithms to recommend movies but don’t trust them to warn us about deadly drug combos. The fact that only 63% of EHR systems properly grade interaction severity is a scandal. It’s not just negligence - it’s systemic failure. We’ve digitized healthcare but kept the mindset of a 1980s doctor’s office.
And yet, the real solution isn’t better tech - it’s better communication. People don’t tell doctors about their CBD oil because they think it’s ‘not medicine.’ But it is. It’s pharmacology in a bottle. We need to reframe how we talk about everything we put in our bodies - not as ‘supplements’ or ‘remedies,’ but as active chemical agents with consequences.
It’s not paranoia. It’s precision.
Nader Bsyouni
December 26, 2025 AT 22:04So we’re supposed to fear every pill and juice and herb like it’s a cult leader whispering poison in our ears? I’ve been on 7 meds for 12 years and I’m still standing. Maybe the problem isn’t the drugs - it’s the fear-mongering. You people act like your body is a bomb that’ll go off if you breathe wrong. Chill. Your liver isn’t that fragile. You’re not a lab rat.
And why do we treat pharmacists like oracles? They’re not doctors. They read labels. I’d rather trust my own experience than some app that flags ‘possible interaction’ because I took ibuprofen with tea.
Stop scaring people. Start trusting them.
Julie Chavassieux
December 27, 2025 AT 21:10Just got back from the ER. Didn’t know I was having serotonin syndrome until my hands wouldn’t stop shaking. Took two different cough meds because I was ‘so sick’ and didn’t realize one had dextromethorphan. My SSRI was already in my system. I thought it was anxiety. Turns out, I was one step from a seizure.
Now I carry my meds in a little ziplock. No more guessing. No more ‘I think I took it.’
Don’t be me.
Jeremy Hendriks
December 28, 2025 AT 14:15You’re all acting like drug interactions are some new invention. They’ve been killing people since the first herbalist mixed foxglove with honey. The real issue? We’ve outsourced our responsibility to apps and pharmacists. You think your phone is going to save you? It’s not. Your brain is. Learn your meds. Know what they do. Read the damn leaflet. Stop treating your body like a black box. You’re not a passenger - you’re the driver. And if you don’t know how the engine works, you shouldn’t be behind the wheel.
Stop waiting for permission to be responsible. Be responsible.
Vikrant Sura
December 29, 2025 AT 21:06So what? People die. That’s life. You think the world cares if some old lady mixes her blood thinner with garlic pills? We got bigger problems. Climate change. Inflation. War. This is just noise. Why are you even reading this? Go outside.