Hypercalcemia Risk Calculator
Risk Assessment Tool
This tool calculates your risk of developing hypercalcemia when taking vitamin D supplements with thiazide diuretics. Based on current medical guidelines and research.
Your calculated risk of hypercalcemia:
When you take vitamin D supplements and a thiazide diuretic together, you might not realize you're putting yourself at risk for something serious: hypercalcemia. It’s not a common problem for everyone, but if you’re on hydrochlorothiazide or chlorthalidone for high blood pressure and also popping daily vitamin D pills-especially doses above 2,000 IU-you could be setting yourself up for trouble.
How Vitamin D and Thiazide Diuretics Work Together (and Why That’s Dangerous)
Vitamin D doesn’t just help your bones. Its active form, calcitriol, tells your intestines to absorb more calcium from food. That’s good if you’re deficient. But when your body already has enough calcium, extra absorption becomes a problem.
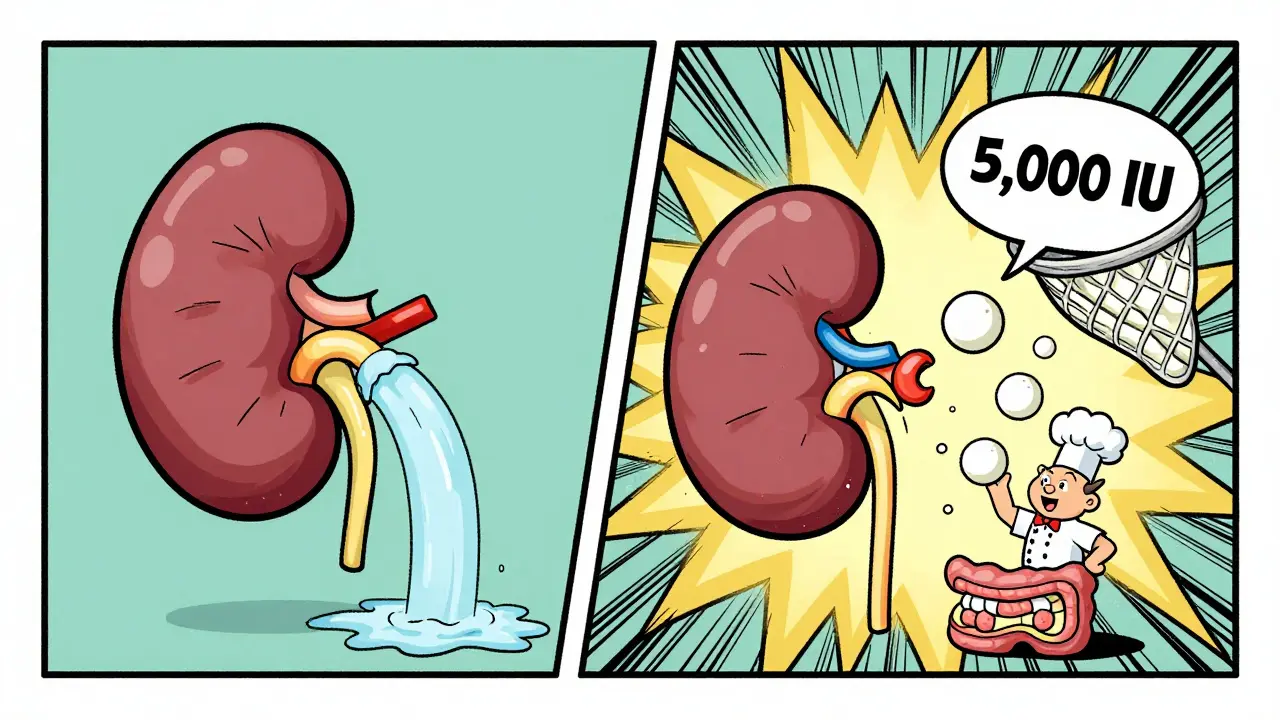
Thiazide diuretics like hydrochlorothiazide (Microzide) and chlorthalidone are designed to help your kidneys get rid of extra sodium and water. But they do something unexpected: they make your kidneys hold onto calcium instead of flushing it out. Studies show they reduce urinary calcium loss by 30-40%. That’s why they’re sometimes used to treat kidney stones-they keep calcium from building up in the urine.
Put them together, and you’ve got a double hit: more calcium comes in through your gut, and less leaves through your kidneys. The result? Your blood calcium levels can creep up. That’s hypercalcemia. And while mild cases might feel like nothing more than fatigue or constipation, severe cases can lead to confusion, kidney damage, heart rhythm problems, and even hospitalization.
Who’s Most at Risk?
This isn’t a risk for everyone. The real danger hits people who:
- Take high-dose vitamin D supplements (5,000 IU or more daily)
- Are over 65 years old
- Have kidney issues or a history of kidney stones
- Take thiazides long-term (more than 6 months)
- Don’t get their calcium levels checked regularly
A 2021 study from the Mayo Clinic found that people on high-dose vitamin D (over 4,000 IU/day) while taking thiazides had an 8-12% chance of developing hypercalcemia. That’s four times higher than those on thiazides alone. And in patients over 65, nearly 22% of hypercalcemia cases were linked to this combo, according to Medicare data.
Here’s the scary part: 61% of seniors on thiazides don’t even know they should be monitoring their calcium levels when taking vitamin D. Many assume supplements are harmless. They’re not.
What Do the Experts Say?
There’s disagreement among doctors, but the trend is clear: caution is needed.
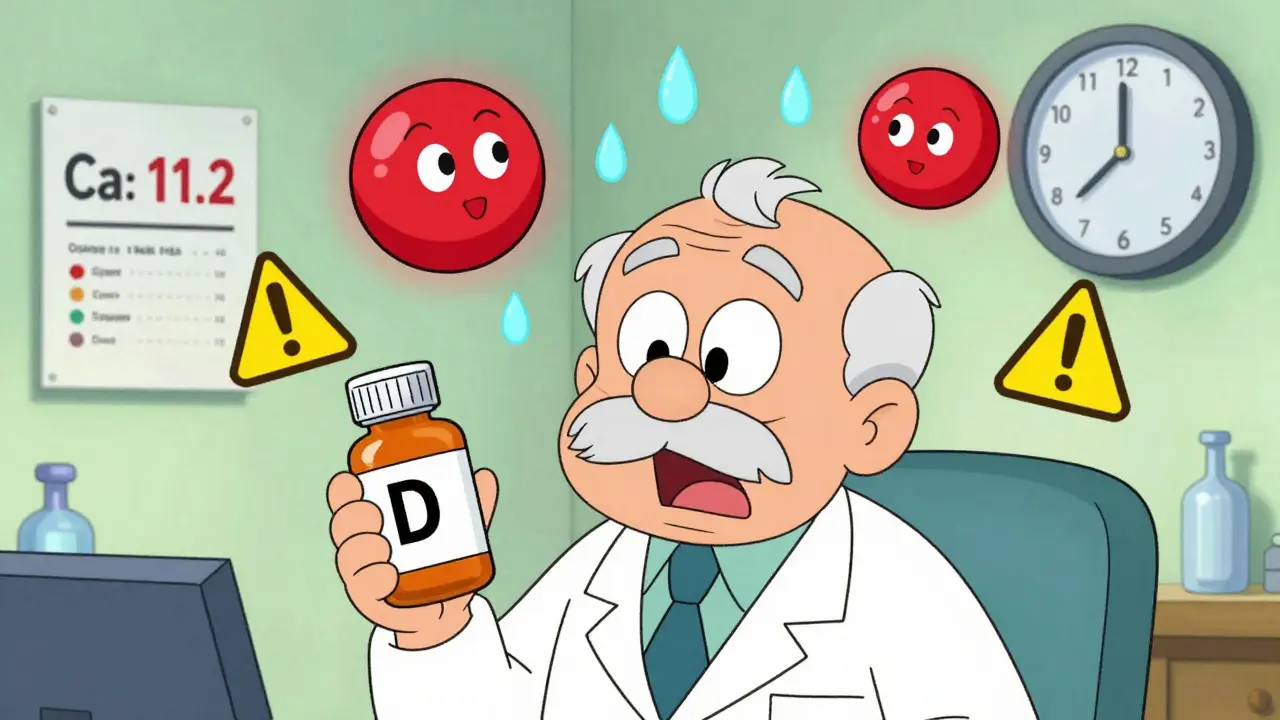
Some, like Dr. Murray Epstein, argue the risk is overstated. He points to studies showing only 0.8% of monitored patients develop serious hypercalcemia. But others, like Dr. John Burnett from Mayo Clinic, call this one of the most underrecognized causes of drug-induced hypercalcemia in older adults. He’s seen too many cases where patients were taking OTC vitamin D3 at 5,000 IU daily with their blood pressure pill-and ended up with calcium levels over 11 mg/dL (normal is 8.5-10.2).
The European Society of Cardiology recommends capping vitamin D at 2,000 IU/day if you’re on thiazides. The American Geriatrics Society Beers Criteria outright calls this combination potentially inappropriate for people with already elevated calcium levels (above 10.2 mg/dL).
And it’s not just guidelines. Real people are reporting it. On Reddit’s r/Pharmacy, 78% of 142 respondents who took high-dose vitamin D with thiazides experienced symptoms like fatigue, nausea, or constipation. One nurse practitioner shared: “I’ve had 3 patients in 6 months with calcium over 11 mg/dL from OTC vitamin D3 and HCTZ-all needed hospitalization.”
What About Other Diuretics?
Not all diuretics act the same. Loop diuretics like furosemide (Lasix) actually make you lose more calcium through urine-so they’re safer if you’re taking vitamin D. Potassium-sparing diuretics like spironolactone don’t affect calcium much either.
But thiazides are still the go-to for most doctors because they lower blood pressure better over 24 hours than alternatives. In fact, 68% of primary care doctors still choose them first, even knowing the risk.
If you’re on a thiazide and need vitamin D, switching diuretics isn’t always practical. But knowing your options matters. If your doctor prescribes a thiazide and you’re already on high-dose vitamin D, ask: “Could a different diuretic work for me?”
What’s the Safe Way to Take Both?
You don’t have to stop vitamin D. You just need to do it right.
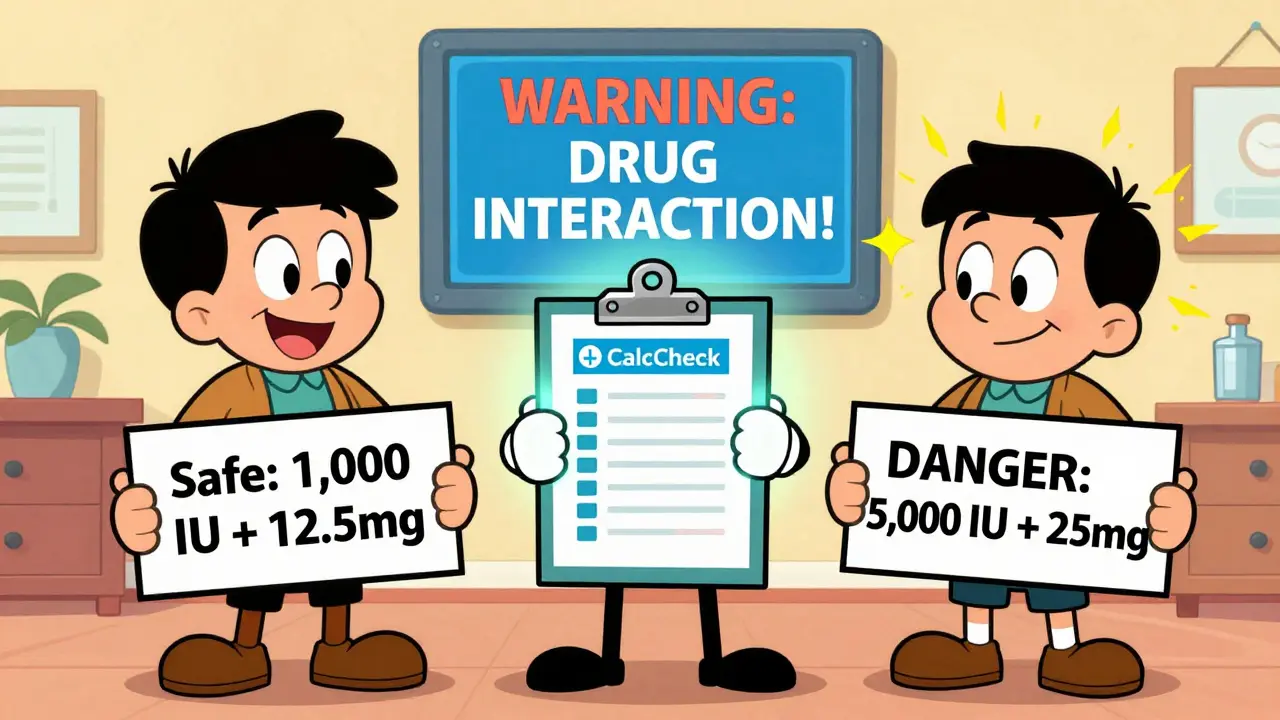
The safest approach, backed by the American Society of Nephrology and Endocrine Society, is:
- Start with the lowest effective dose of vitamin D-800 to 1,000 IU daily. That’s enough for most people to maintain bone health without raising calcium.
- Use the lowest effective thiazide dose. Instead of 25 mg of hydrochlorothiazide, try 12.5 mg. It still lowers blood pressure, but with less calcium retention.
- Get your serum calcium tested before starting both, then again at 3 months, and every 6-12 months after that.
- Ask your doctor to check your albumin level too. Calcium in the blood binds to albumin. If your albumin is low, your total calcium might look high even if your “free” calcium is normal. A corrected calcium level gives the real picture.
- Don’t take more than 2,000 IU of vitamin D daily unless your doctor specifically tells you to-and even then, monitor closely.
A 2022 study showed that when pharmacists actively monitored patients on this combo and adjusted doses, hypercalcemia dropped from 11.3% to just 2.7%. Simple interventions make a huge difference.
What Should You Do Right Now?
If you’re taking a thiazide diuretic and vitamin D, here’s what to do immediately:
- Check your vitamin D supplement label. If it’s 2,000 IU or higher, talk to your doctor.
- Look up your last blood test results. Was your calcium checked? When?
- Write down any symptoms: fatigue, frequent urination, nausea, constipation, confusion, or muscle weakness. These can be early signs.
- Don’t stop your medications. But do schedule a visit with your doctor to review your regimen.
Many people think supplements are safe because they’re “natural.” But vitamin D is a hormone precursor. At high doses, it acts like a drug. And when combined with thiazides, it can push your body past its limit.
What’s New in 2026?
There’s progress on the horizon. In 2023, the FDA approved a new test called CalcCheck that looks at your genetic variants in the calcium-sensing receptor gene. It can predict whether you’re more likely to develop hypercalcemia from this combo. It’s not widely used yet, but it’s coming.
Also, newer thiazide-like drugs like metolazone may have less calcium-sparing effect-only about 25% reduction compared to 35-42% for traditional thiazides. That could mean safer options down the road.
And health systems like Kaiser Permanente are already using electronic alerts in their patient records. If you’re prescribed vitamin D over 2,000 IU while on a thiazide, your doctor gets a warning. That’s cut inappropriate combinations by 63%.
Bottom Line
You can take vitamin D and a thiazide diuretic safely-but only if you’re smart about it. The risk of hypercalcemia is real, especially for older adults and those on high-dose supplements. But it’s preventable.
Low-dose vitamin D (800-1,000 IU) + low-dose thiazide (12.5 mg hydrochlorothiazide) + regular calcium checks = safe. High-dose vitamin D + standard thiazide + no monitoring = dangerous.
Don’t assume your doctor knows about this interaction. Many don’t. Only 42% of internists know how often to check calcium levels in these patients. Be your own advocate. Ask for a blood test. Ask about your dose. Ask if there’s a safer alternative.
This isn’t about avoiding treatment. It’s about using it wisely. Your bones need vitamin D. Your blood pressure needs a diuretic. But your body needs balance. And that balance starts with knowing the risk-and acting on it.




Mindee Coulter
January 27, 2026 AT 12:41Just took my HCTZ and 5000 IU D3 this morning. Guess I’m gonna get a blood test this week. Thanks for the wake-up call.
Colin Pierce
January 28, 2026 AT 05:44Real talk: most docs don’t even know this interaction. I’m a pharmacist and I’ve seen 3 patients in 6 months with calcium over 11 from this combo. No symptoms until they were confused and dehydrated. Check your labs. Seriously.
Anna Lou Chen
January 28, 2026 AT 18:29Let’s not moralize nutrient metabolism as if it’s a neoliberal conspiracy. The calcium-sensing receptor is a G-protein-coupled evolutionary adaptation, not a pharmaceutical plot. When you pharmacologically inhibit renal calcium excretion while exogenously upregulating intestinal absorption via calcitriol-mediated TRPV6 translocation, you’re not ‘being careless’-you’re engaging in a pharmacokinetic cascade with non-linear thresholds. The 8-12% hypercalcemia rate isn’t ‘dangerous’-it’s statistically significant in a population with low baseline variability. We need population-level pharmacovigilance, not fear-mongering.
Also, why is everyone assuming vitamin D is a supplement? It’s a prohormone. You wouldn’t say ‘I’m just taking estrogen’ while on an ACE inhibitor.
Mark Alan
January 30, 2026 AT 10:28USA: 68% of docs still prescribe HCTZ. Canada: banned high-dose D3 without a prescription. Europe: capped at 2K IU. Meanwhile, I’m over here buying 10K IU gummies from Amazon because ‘natural’ 😭
AMERICA, WE ARE THE PROBLEM. 🇺🇸💀
Ambrose Curtis
January 31, 2026 AT 02:12my grandma took 5000iu d3 + hctz for 2 years and never had a problem. she’s 81 and still walks 3 miles a day. maybe it’s not that bad? also, why are we blaming the meds and not the fact that people take way too much d3? i mean, come on. it’s not like we’re talking about chemo here.
also, my doc never checked my calcium. i had to ask. now i get it checked every 6 months. easy fix.
Linda O'neil
January 31, 2026 AT 17:54You’re not alone. I started this combo 8 months ago. Felt tired, constipated, thought it was just aging. Got my levels checked after reading this-calcium was 10.9. Doctor was shocked. We dropped my D3 to 1000 IU and switched to a loop diuretic. Energy’s back. I’m alive again. Don’t wait until you’re in the ER.
James Dwyer
February 2, 2026 AT 08:06This is exactly the kind of info that should be in every pharmacy pamphlet. Thank you for writing this. I’m sharing it with my mom. She’s on HCTZ and takes D3 ‘just in case.’
jonathan soba
February 3, 2026 AT 13:47Interesting that the Mayo Clinic study is cited, yet the sample size isn’t disclosed. Also, 78% of Reddit respondents? That’s not data, that’s confirmation bias. And why are we ignoring the confounding variable of obesity? Adipose tissue stores vitamin D-higher BMI = higher baseline D3 = lower incremental risk. Also, the 2022 study on pharmacist intervention-was it randomized? Controlled? Double-blind? Or just a convenience sample from one clinic? The data is suggestive, not conclusive.
Phil Davis
February 4, 2026 AT 14:35So let me get this straight. The solution to a drug interaction is… more doctor visits? More blood tests? More paperwork? And we wonder why people don’t take their meds.
Meanwhile, the FDA approved a genetic test that costs $800 and isn’t covered by insurance. Brilliant. Just brilliant.
Irebami Soyinka
February 5, 2026 AT 00:50My people in Lagos? They don’t even know what vitamin D is. They get sunlight, they eat fish, they live to 90. Meanwhile, Americans take 10K IU pills and wonder why they’re tired. 😂
Stop buying supplements like they’re candy. Your body isn’t a vending machine. 🌞💊
doug b
February 6, 2026 AT 22:41Low dose D3 + low dose HCTZ + yearly blood test = you’re golden. No need to panic. Just be smart. Your body’s not broken. You just need to tune it.
Mel MJPS
February 6, 2026 AT 23:08I’m so glad I read this. I’ve been taking 5000 IU since 2020. My doctor never mentioned this. I’m calling them tomorrow. Thank you for sharing.
Katie Mccreary
February 7, 2026 AT 13:26So… you’re saying I can’t just take my gummy and my blood pressure pill and pretend everything’s fine? 😭
SRI GUNTORO
February 9, 2026 AT 12:17This is what happens when people forget the wisdom of our ancestors. We didn’t have labs or pills. We had sun. We had food. Now we’re drowning in supplements and bad science. Shame.
Kevin Kennett
February 10, 2026 AT 03:03Look, I get it. You’re scared. I’ve been there. But don’t freak out. Talk to your doctor. Get your calcium checked. Maybe lower your D3. Maybe switch to a different diuretic. It’s not about fear. It’s about awareness. You’re not weak for asking questions. You’re smart. And you’re not alone.