Type 1 diabetes isn't just about high blood sugar. It's an autoimmune war happening inside the pancreas, where the body's own immune system attacks and kills the insulin-producing beta cells. This isn't a slow decline-it's a targeted destruction that leaves the body with almost no ability to make insulin. Without insulin, glucose can't enter cells for energy, and the body starts breaking down fat, leading to dangerous conditions like diabetic ketoacidosis. This isn't a lifestyle issue. It's not caused by eating too much sugar. It's an autoimmune disease, and managing it means understanding the biology behind the attack.
How the Immune System Turns Against the Pancreas
The pancreas doesn’t just make insulin. It has clusters of cells called islets, and inside those islets are beta cells. These cells are the only ones in the body that produce insulin. In type 1 diabetes, the immune system misidentifies these beta cells as foreign invaders. T-cells, which are supposed to protect you from viruses, instead swarm the islets and destroy them. This process, called insulitis, can start years before anyone notices symptoms.Researchers have found specific targets the immune system goes after: insulin itself, GAD65, IA-2, and ZnT8. These are proteins inside the beta cells. When the body makes antibodies against them-called islet autoantibodies-it’s a clear sign the autoimmune attack is underway. Blood tests for these antibodies can detect type 1 diabetes before symptoms appear. That’s why some kids with a family history get screened. Finding these antibodies early means you might catch the disease in Stage 1 or Stage 2, before full-blown diabetes kicks in.
Genetics play a big role. People with HLA-DR3 or HLA-DR4 gene variants have a 20 to 30 times higher risk. But genes alone don’t cause it. Something triggers the attack. Viruses, especially coxsackievirus B, are suspected culprits. Studies show people who later develop type 1 diabetes often had enterovirus infections months before diagnosis. Environmental factors like diet, gut health, and even vitamin D levels might influence how the immune system reacts. The exact trigger isn’t known yet, but the evidence points to a mix of genes and environment.
Stages of Type 1 Diabetes: Before Symptoms Show
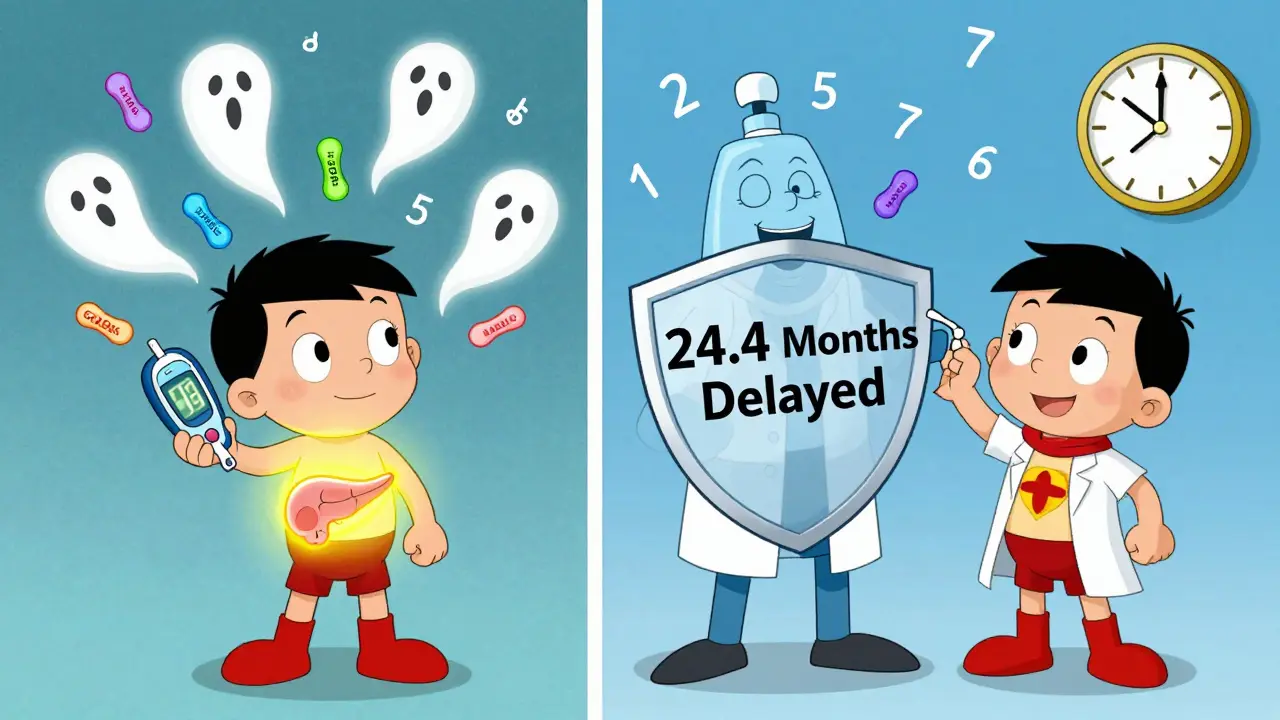
Type 1 diabetes doesn’t just appear overnight. The TrialNet consortium defined three clear stages:- Stage 1: Two or more autoantibodies are present, but blood sugar is still normal. No symptoms. This stage affects about 0.4% of the general population.
- Stage 2: Autoantibodies are still there, but now blood sugar is starting to rise. Still no symptoms. About 0.15% of people are here.
- Stage 3: Symptoms appear-excessive thirst, frequent urination, weight loss. Blood sugar is high. Insulin is now required.
This staging system changes everything. It means you can intervene before someone needs insulin. That’s where teplizumab (Tzield) comes in. It’s the first FDA-approved drug that can delay the onset of Stage 3. In the PROTECT trial, it pushed back diagnosis by nearly 2.5 years on average. That’s not a cure, but it’s a massive win. More time without insulin means more time for the body to hold onto its own beta cells.
Why Insulin Alone Isn’t Enough
People with type 1 diabetes need insulin. That’s non-negotiable. But insulin therapy doesn’t fix the autoimmune attack. It just replaces what’s been lost. That’s why many people still struggle with blood sugar swings, hypoglycemia, and long-term complications.Modern insulin therapy is far more precise than it used to be. Rapid-acting analogs like insulin aspart or lispro mimic meals better. Long-acting insulins like glargine U-300 last longer and have fewer peaks. Most people now use multiple daily injections (MDI) or insulin pumps. But even the best insulin can’t perfectly mimic a healthy pancreas. That’s why continuous glucose monitors (CGMs) like the Dexcom G7 are now standard. These devices give real-time data, alerting you when blood sugar is dropping or rising too fast. Studies show CGMs reduce HbA1c by 0.4% to 0.6% and cut hypoglycemic events by nearly half.
Then there’s the closed-loop system-the “artificial pancreas.” Devices like Tandem’s Control-IQ automatically adjust insulin delivery based on CGM readings. In one 2022 JAMA study, users spent 71-74% of their time in the target glucose range (70-180 mg/dL). That’s a huge jump from 51-55% with traditional pumps. For parents of kids with type 1, this means fewer nighttime alarms and more sleep. For adults, it means less mental load.
The Hidden Connection: Autoimmune Pancreatitis and Type 1 Diabetes
Most people don’t realize type 1 diabetes can be part of a bigger autoimmune picture. In rare cases-about 1 in 300-people with type 1 diabetes also develop autoimmune pancreatitis (AIP). This is a different condition. Instead of attacking the insulin-producing islets, the immune system attacks the exocrine pancreas-the part that makes digestive enzymes.AIP has two types. Type 1 is linked to high levels of IgG4 antibodies and often responds well to steroids. Type 2 is tied to inflammatory bowel disease. When both conditions happen together, it’s a red flag. The patient might have abdominal pain, bloating, or malabsorption-symptoms that look nothing like typical diabetes. If a person with type 1 diabetes suddenly has trouble digesting food or losing weight despite eating enough, doctors need to check for AIP. A simple blood test for IgG4 and an MRI of the pancreas can reveal it.
Managing both conditions is tricky. Steroids used for AIP can spike blood sugar, sometimes requiring a 30-50% increase in insulin doses. That’s why endocrinologists and gastroenterologists need to work together. The 2023 ADA guidelines now recommend checking for pancreatic enzyme deficiency in type 1 patients with persistent GI symptoms. About 5-10% of long-term type 1 patients develop this. Enzyme replacement therapy can restore digestion and prevent nutrient loss.
Emerging Therapies: Beyond Insulin
The future of type 1 diabetes isn’t just better insulin-it’s stopping the immune attack and saving beta cells.Teplizumab was the first breakthrough, but it’s only for Stage 2. Other drugs are in the pipeline. Abatacept, originally used for rheumatoid arthritis, slowed beta-cell decline by 59% in recent-onset type 1 patients over two years. Verapamil, a blood pressure medication, showed surprising promise in a 2022 Cell Metabolism trial: patients preserved 30% more of their own insulin production after 12 months. It’s not a miracle cure, but it’s a step.
Then there’s stem cell therapy. Vertex Pharmaceuticals’ VX-880 trial gave 12 people with type 1 diabetes lab-grown islet cells. At 90 days, 89% were insulin-free. Not all of them stayed that way long-term, but it’s proof the body can accept new, functional beta cells. The next phase will test larger groups and longer outcomes.
Even the gut microbiome is getting attention. A 2022 Nature Microbiology study found that people with type 1 diabetes have less of a beneficial gut bacteria called Faecalibacterium prausnitzii. This bug produces butyrate, which helps calm inflammation. Early trials are testing probiotics and fiber supplements to see if changing gut bacteria can slow disease progression.

What This Means for Daily Life
Managing type 1 diabetes today is more complex than ever-but also more manageable. You need to think beyond blood sugar numbers. You need to consider:- Is your insulin delivery system working? Are you using a CGM or pump?
- Have you been tested for autoantibodies if you’re at risk?
- Do you have unexplained GI symptoms? Could it be autoimmune pancreatitis?
- Are you aware of new therapies like teplizumab if you’re in Stage 2?
- Is your care team including both an endocrinologist and, if needed, a gastroenterologist?
Insulin is still the foundation. But now, the goal is to preserve what’s left of the pancreas, delay complications, and improve quality of life. That means staying informed, asking questions, and working with a team that understands the full scope of this autoimmune disease.
Key Numbers to Remember
- 1.25 million Americans live with type 1 diabetes (2023 ADA data).
- Less than 5% of normal insulin production remains at diagnosis.
- Teplizumab delays diagnosis by 24.4-29.8 months on average.
- CGMs reduce HbA1c by 0.4-0.6% and cut hypoglycemia by 40-50%.
- Artificial pancreas systems achieve 71-74% time-in-range.
- 89% of participants in Vertex’s VX-880 trial became insulin-free at 90 days.
- 5-10% of long-term type 1 patients develop pancreatic enzyme deficiency.
Can type 1 diabetes be reversed?
No, type 1 diabetes cannot be reversed yet. The immune system has already destroyed most of the insulin-producing beta cells. However, new therapies like teplizumab can delay progression, and stem cell transplants have restored insulin production in some patients. These aren’t cures, but they’re steps toward functional recovery. The focus now is on preserving remaining beta cells and protecting new ones.
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes attacks the endocrine pancreas (islet cells that make insulin). Autoimmune pancreatitis attacks the exocrine pancreas (cells that make digestive enzymes). They are separate diseases, but they can happen together in rare cases. When they do, it’s called a broader autoimmune pancreatic syndrome. Diagnosis requires different tests: autoantibodies for type 1 diabetes, IgG4 levels and imaging for autoimmune pancreatitis.
Why do some adults with type 1 diabetes get misdiagnosed as type 2?
Because type 1 diabetes in adults-sometimes called LADA (Latent Autoimmune Diabetes in Adults)-progresses slowly. These patients may still produce a little insulin, look overweight, and respond to oral meds at first. But they’ll eventually need insulin. Studies show 12% of adults with type 1 are initially misdiagnosed as type 2, leading to delayed insulin therapy. Testing for autoantibodies (GAD65, IA-2) can prevent this mistake.
How do I know if I’m in Stage 1 or Stage 2 of type 1 diabetes?
You need a blood test. Stage 1 means you have two or more islet autoantibodies (like GAD65 or ZnT8) but normal blood sugar. Stage 2 means those same antibodies are present, but your blood sugar is starting to rise-still no symptoms. These stages are usually found in people with a family history of type 1 diabetes or through research programs like TrialNet. Routine screening isn’t common, but if you’re at risk, ask your doctor about antibody testing.
Can diet or supplements cure type 1 diabetes?
No. No diet, supplement, or alternative therapy can cure type 1 diabetes. While a healthy diet helps manage blood sugar, and some studies look at vitamin D or omega-3s for immune modulation, none have proven to stop the autoimmune attack. Be wary of claims that promise a cure. The only proven treatments are insulin, CGMs, insulin pumps, teplizumab (for Stage 2), and emerging therapies like stem cell transplants-all under medical supervision.