When your child has a rash, eczema flare-up, or teething discomfort, it’s tempting to reach for a cream or ointment right away. But what seems like a quick fix can turn dangerous if you don’t know how to use topical medications safely in children. Unlike adults, kids absorb medicine through their skin much more easily - sometimes three to five times more. For babies under one year, that number can jump even higher. A little too much, applied too often, or left within reach, and what was meant to help can land your child in the emergency room.
Why Children’s Skin Is Different
Children’s skin isn’t just smaller skin - it’s built differently. Their outer layer, called the stratum corneum, is thinner. Their surface-area-to-body-weight ratio is much higher. That means a cream spread over a small patch of skin can end up in their bloodstream faster and in greater amounts than you’d expect. Infants, especially, have skin that’s still developing its natural barrier. This makes them more vulnerable to side effects from even mild medications.For example, applying a standard dose of hydrocortisone cream to a 10-pound baby over 20% of their body - say, both arms and legs - can have the same hormonal effect as giving them an oral steroid. That’s not theoretical. It’s been documented in medical studies. And it’s why doctors stress using the lowest strength possible for the shortest time.
What to Avoid Completely
Some topical products have no place in a child’s medicine cabinet. The FDA has banned benzocaine-containing teething gels and sprays for children under two because they can cause methemoglobinemia - a rare but life-threatening condition where the blood can’t carry oxygen properly. Symptoms show up fast: bluish lips or skin, rapid breathing, drowsiness. In documented cases, oxygen levels dropped below 80% within 30 minutes of application.Same goes for dibucaine and other strong topical anesthetics. These aren’t just risky - they’re unnecessary. Chilled (not frozen) teething rings, gentle gum massage, or a cold washcloth work just as well without the danger. There’s no need to risk a child’s life for a few minutes of comfort.
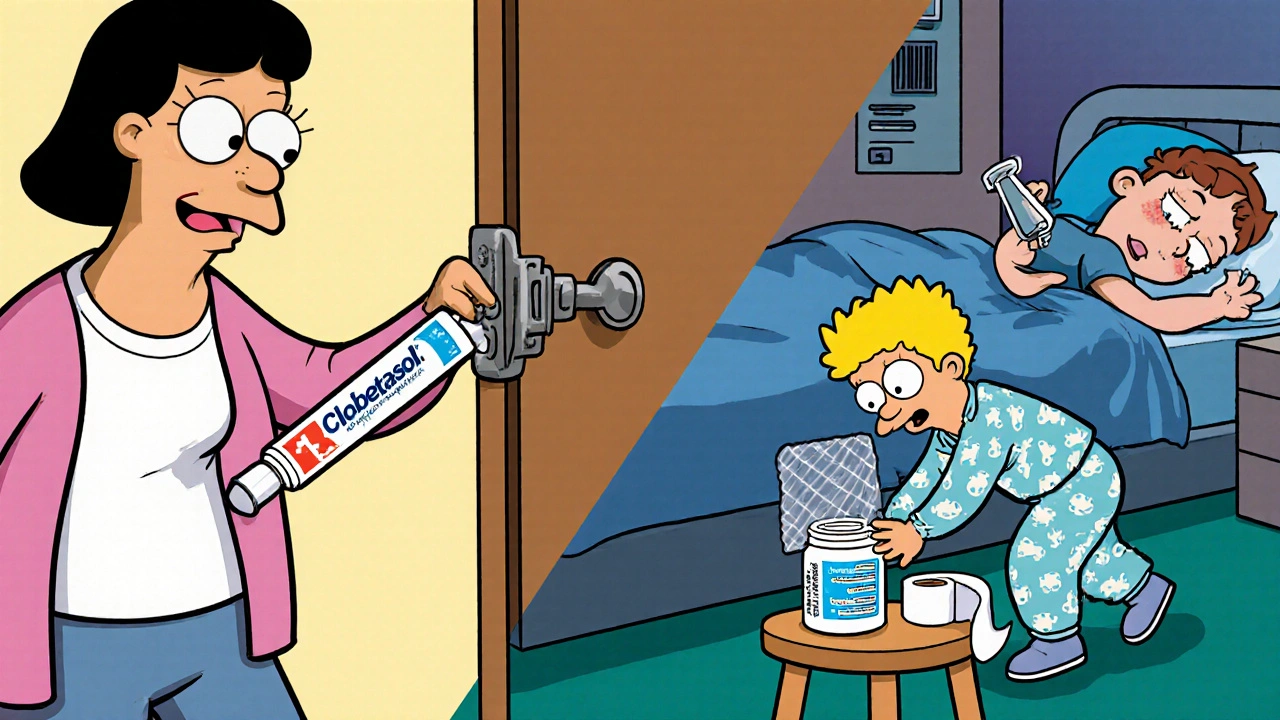
Also avoid potent corticosteroids - like clobetasol or betamethasone - on children under two. These are class I or II steroids, the strongest available. Even short-term use can suppress the adrenal glands, which control stress response and metabolism. A 2022 review of over 12,000 pediatric patients found that 15.8% of those using high-potency steroids developed signs of adrenal suppression, compared to just 2.3% using mild ones.
What’s Safe - and How to Use It Right
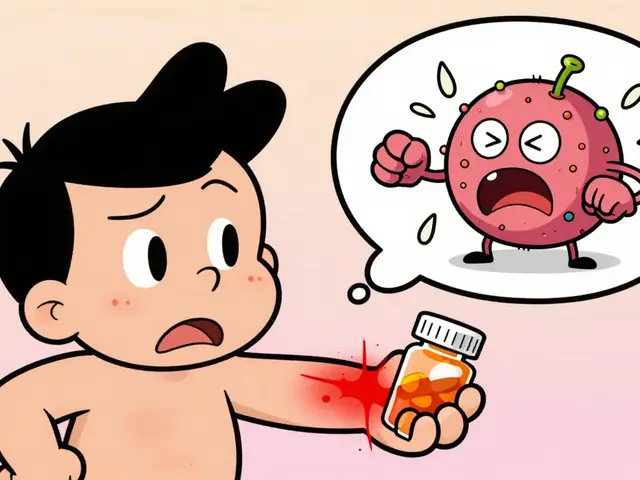
Not all topical meds are dangerous. Many are essential for managing eczema, diaper rash, or minor infections. But safety comes down to three things: the right product, the right amount, and the right application.For mild eczema or dry skin, over-the-counter hydrocortisone 0.5% or 1% is usually fine for kids over two. For infants as young as three months, non-steroidal options like tacrolimus 0.03% or pimecrolimus are approved and show 72% less systemic absorption than even low-dose steroids. These are often preferred for the face and neck, where steroid use carries higher risk.
For pain relief during minor procedures - like a shot or IV insertion - lidocaine cream can be used safely, but only under guidance. It should be applied 30 to 60 minutes before the procedure, covered with a bandage (occlusion), and never used on broken skin. The maximum dose for children under three is 1.2 grams total in 24 hours. That’s about two fingertip units (FTUs) for a small area.
What’s a fingertip unit? It’s the amount of cream squeezed from a standard tube, from the tip of your index finger to the first crease. One FTU covers an area about the size of two adult palms. For a 10kg child, you shouldn’t use more than two FTUs per day - and never on more than 10% of their body surface at once.

Occlusion: The Hidden Danger
Many parents think covering a cream with plastic wrap or a Tegaderm dressing helps it work better. It does - too well. Occlusion can boost absorption by 300% to 500%. For a child with eczema, whose skin is already inflamed and more porous, this can be deadly. One study showed absorption through damaged skin can jump from 3% to 60% for lidocaine. That’s why doctors warn against wrapping kids in plastic after applying steroid creams, even if it’s meant to soothe the rash.If your child’s doctor recommends occlusion for a specific condition - like severe psoriasis or stubborn eczema - they’ll give exact instructions on how long to leave it on and how often. Never do it on your own.
Storage and Prevention of Accidental Ingestion
Most pediatric topical medication emergencies happen because the product was left out. According to the American Association of Poison Control Centers, 78% of exposures occur when parents forget to put the tube back in the cabinet after use. That’s not negligence - it’s human. You’re tired. You’re holding your baby. You just squeezed out a bit of cream and set the tube down.Here’s what you need to do: Every time you use a topical medication - even if it’s just a drop - put it back in its child-resistant container and lock it away. Out of sight, out of reach. Not on the bathroom counter. Not on the changing table. Not in your purse. Keep it in a high cabinet, preferably one with a latch.
Also, never share medications. Grandparents, aunts, or friends might offer you their leftover hydrocortisone cream. Don’t take it. The strength, expiration date, and intended use might be wrong for your child. A 2023 survey found 19% of households share topical meds - and it’s one of the top reasons for accidental overdoses.
Recognizing Trouble - When to Call for Help
Most side effects happen slowly. But some come on fast. If your child shows any of these signs after using a topical medication, seek help immediately:- Bluish or grayish skin, especially around the lips or fingernails (sign of methemoglobinemia)
- Drowsiness, confusion, or trouble waking up
- Shaking, seizures, or irregular heartbeat
- Difficulty breathing or rapid breathing
- Swelling of the face, lips, or tongue
Methemoglobinemia from benzocaine requires urgent treatment with methylene blue. Lidocaine toxicity can cause seizures and needs IV support. Don’t wait. Call poison control (1-800-222-1222) or go to the ER.
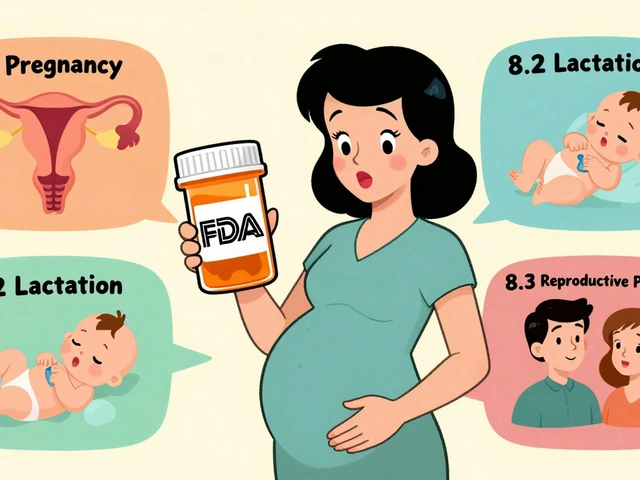
What’s Changing - And What to Watch For
The FDA is pushing for better labeling on all topical medications. By 2026, new products should clearly state: age limits, maximum daily dose, body surface area restrictions, and duration guidelines. Right now, only 37% of over-the-counter topical pain relievers include child-specific instructions.Also, new delivery systems are coming. Nanoparticle-based creams are in late-stage trials and promise to cut systemic absorption by 70-80% while keeping the skin benefits. These could be game-changers for eczema care.
Meanwhile, some companies are adding QR codes to packaging. Scan it, and you get a short video on safe use for kids - no more guessing.
Bottom Line: Less Is More
The golden rule for topical medications in children is simple: use the weakest effective product, for the shortest time, on the smallest area possible. Don’t apply more because you think it’ll work faster. Don’t use adult products because they’re “close enough.” Don’t leave them out because you’re in a hurry.When in doubt, ask your pediatrician or pharmacist. They can help you pick the right product and show you how much to use. And remember - for teething, a cold cloth works better than any gel. For eczema, moisturizing daily is often more effective than steroids. Safe doesn’t mean fancy. It means smart.



rob lafata
November 20, 2025 AT 15:53Let me guess - you’re one of those parents who thinks ‘natural’ means ‘safe’? Cool. So you’re fine with letting your kid scream for hours while their eczema oozes like a swamp monster? I’ve seen moms slap coconut oil on a raw, bleeding patch and call it ‘holistic.’ Spoiler: it’s not. Hydrocortisone 1% is not poison. It’s medicine. Used right. Not like that weird tea tree oil paste you smeared last week - yeah, I saw your Instagram story. You’re not a healer. You’re a liability.
And don’t even get me started on the ‘cotton swab with honey’ crowd. Honey is not a topical steroid. It’s a bacterial buffet. Your kid’s skin isn’t a yoga retreat. It’s a biological interface. Treat it like one.
Also - stop sharing creams. That’s not ‘sharing is caring.’ That’s ‘I’m a walking CDC case study.’
Matthew McCraney
November 21, 2025 AT 09:20ok so here’s the real story no one wants to tell u… the fda is in bed with big pharma and they banned benzocaine because they want you to buy their $$$ steroid creams instead. they dont care if your baby is in pain. they care about profits. i read on a forum that methemoglobinemia is RARE like less than 1 in 100k cases but they make it sound like every kid will die. its fearmongering. why do u think all the ‘safe’ alternatives are so expensive? coincidence? i think not.
also my cousin used benzocaine gel on her 11mo old and she lived. so did her dog. so chill out.
and who says you cant use clobetasol on a baby? my uncle was a nurse in the 80s and he said they used it all the time. they just didn’t have lawyers then.
the real danger? trusting doctors who get paid by drug reps. ask yourself: who funds the ‘guidelines’?
serge jane
November 23, 2025 AT 02:51There’s something deeply human about wanting to fix pain quickly. Especially when it’s your child. We’re wired to act - to reach for something, anything - when we see them uncomfortable. But medicine isn’t about speed. It’s about respect. For the body’s delicate balance. For the fact that skin isn’t just a container. It’s a living filter. A gatekeeper. A teacher.
Children aren’t small adults. They’re developing systems. And every molecule we push through that thin barrier echoes through their entire being. That’s not just science. It’s sacred. The fact that we’ve forgotten that - that we treat skin like a sponge to soak up quick fixes - says more about our culture than our medicine.
Maybe the real problem isn’t the creams. It’s our impatience. Our fear of discomfort. Our refusal to sit with the quiet. To hold a cold cloth. To breathe with them. To wait.
There’s power in restraint. In saying no. Even when it’s hard. Even when everyone else is reaching for the tube.
And yes - locking it away? That’s not paranoia. That’s love.
Just because something works doesn’t mean it’s right. And just because it’s legal doesn’t mean it’s wise.
Nick Naylor
November 24, 2025 AT 21:46Brianna Groleau
November 26, 2025 AT 15:34I’m from a small town in Mississippi and we used to rub Vaseline and a little baby powder on everything - diaper rash, bug bites, even the weird red spot on my cousin’s cheek. My grandma never read a label. She just knew what worked. And guess what? We all turned out fine.
But then I had my daughter. And I started reading. And I realized - we were lucky. We weren’t smart. We just got lucky.
I used to think ‘topical meds’ were just for grown-ups. Then I saw my baby’s face turn red after I put on that ‘gentle’ cream from my mom’s cabinet. I panicked. I called the pediatrician. She didn’t yell. She just said, ‘Let’s start over.’
Now I use the FTU thing. I lock everything up. I don’t use anything without checking the age. I even have a little chart on the fridge. It’s not about being perfect. It’s about being intentional.
And yeah - sometimes I still forget. But now I have a system. And that’s what saves lives. Not fear. Not guilt. Just a little more care.
Rusty Thomas
November 26, 2025 AT 18:07OK BUT DID YOU KNOW that some of these ‘safe’ creams have microplastics in them?? I saw a video on TikTok where they used a UV light and the cream glowed like a zombie. Like… are we just putting plastic on our babies’ skin?? And why is no one talking about this??
Also I heard from a doula that the FDA banned benzocaine because it’s linked to alien abductions. I’m not joking. She said it was in the ‘hidden appendix’ of the 2019 bill. I looked it up. It’s not there. But I still don’t trust them.
My baby uses coconut oil and crystals now. It’s working. I don’t need your ‘FTUs’ or your ‘studies.’ I have vibes. And my vibes say: less chemicals. More earth.
PS: I also don’t vaccinate. But that’s another thread. 😈
Sarah Swiatek
November 27, 2025 AT 22:27Let’s be real - most of these guidelines exist because someone’s kid ended up in the ER after a well-meaning grandma used ‘the same cream I used on my kids in ’87.’
And yeah, the FTCU thing? It’s weird. I thought I was using a pea-sized amount. Turns out I was using a golf ball. I felt like an idiot. Then I bought those little measuring spoons for creams. Now I use them. No shame.
And the occlusion thing? I used to wrap my son’s legs in plastic wrap because the dermatologist said ‘keep it moist.’ Turns out they meant ‘cover with a cotton sock.’ I didn’t ask for clarification. I assumed. Big mistake. His skin turned purple. Not fun.
So yeah - read the label. Ask the pharmacist. Write it down. Don’t assume. Don’t guess. Don’t be the person who says ‘it worked for my cousin.’
Also - the QR code thing? Genius. I scanned one last week. It showed a 45-second video of someone squeezing cream from a tube. I cried. Not because it was sad. Because I realized I’d been doing it wrong for two years.
It’s not about being perfect. It’s about being willing to learn.
Dave Wooldridge
November 28, 2025 AT 09:27They’re lying. All of it. The FDA, the AAP, the ‘experts.’ They want you scared. Why? So you’ll buy their ‘special’ pediatric creams that cost $40 a tube. Meanwhile, the same active ingredient in a $5 adult tube? Identical. Same molecule. Same chemistry.
They say ‘don’t use clobetasol on babies’ - but why? Because they’re scared of lawsuits. Not because it’s dangerous. I’ve got a cousin who used it on his 6-month-old for 3 months straight. Kid’s now 12. Plays soccer. No adrenal issues.
And the ‘fingertip unit’? That’s just a marketing tool to make parents feel like they need a PhD to use lotion.
Here’s the truth: if you use it sparingly, it’s fine. If you don’t, you’re an idiot. But don’t let them gaslight you into thinking every drop is a death sentence.
Also - lock it away? Please. My kid’s 3. He eats crayons. He’s not going to open a childproof cap. He’ll just throw the whole tube on the floor and cry. So I leave it out. He’s fine. We’re fine. You’re the one with the problem.
Rebecca Cosenza
November 30, 2025 AT 00:59Lock it up.
Don’t share.
Use the FTU.
That’s it.
swatantra kumar
December 1, 2025 AT 11:14Bro in India we use neem oil, turmeric paste, and cold rice water for everything. No creams. No labels. No FTUs. My cousin’s baby had eczema for 8 months - we used only coconut oil and a cotton cloth. No steroids. No doctor. He’s 5 now and runs like a cheetah.
Why are we copying American guidelines? We have 5000 years of Ayurveda. Why are we scared of natural? The FDA is just trying to sell you pills.
Also - QR codes? LOL. We just ask the aunty next door. She knows everything.
PS: I used hydrocortisone on my kid once. He cried. I stopped. He’s fine. So maybe less is more. But maybe also… less Western? 🙏
Cinkoon Marketing
December 3, 2025 AT 03:18Interesting. I work in pediatric dermatology marketing and I can tell you that the FTCU system was actually developed by a pharmaceutical consortium in 2018 to standardize dosing for compliance tracking. It’s not a medical innovation - it’s a regulatory tool. Also, the QR code initiative? That’s a new FDA pilot program to reduce liability exposure. Not ‘parent education.’
And the nanoparticle creams? They’re being tested by L’Oréal’s derm division. Not ‘big pharma.’
So… who’s really benefiting here? Not the parents. Not the kids. The system.
robert cardy solano
December 3, 2025 AT 19:15My kid had eczema. We tried everything. Steroids. Oils. Baths with oatmeal. Dead Sea salt. Even a ‘healer’ who chanted over the cream.
Turns out? She just needed a humidifier and to stop wearing wool.
Not a miracle. Not a cure. Just… less irritation.
Maybe the real answer isn’t in the tube. Maybe it’s in the laundry detergent. Or the bathwater temp. Or the fact that we’re wiping her with a rough towel.
So yeah - use the cream if you need to. But don’t forget to look around. The problem might not be what you’re putting on. It’s what you’re putting her in.
Pawan Jamwal
December 4, 2025 AT 08:03India has been using herbal creams for centuries. Why are we listening to American FDA? They banned turmeric paste because it’s ‘unregulated.’ LOL. We use neem, aloe, and honey - all natural, all safe. Your ‘FTU’ is just a scam to sell more expensive products. My son’s rash went away in 2 days with coconut oil. No doctor. No prescription. No fear.
Western medicine is broken. We don’t need your ‘guidelines.’ We need our traditions.
Also - I use clobetasol on my 1-year-old. He’s fine. You’re just scared.
PS: I scanned the QR code. It linked to a YouTube ad for a $50 cream. Classic.
Bill Camp
December 5, 2025 AT 09:39I read this whole thing. Then I went to the bathroom. Pulled out the hydrocortisone. Squeezed out a line. Looked at it. Put it back. Didn’t use it.
Just… didn’t.
My kid’s rash faded on its own. Took 3 days.
I didn’t need the cream.
Maybe the real message isn’t ‘how to use it.’
Maybe it’s ‘when not to.’
Lemmy Coco
December 5, 2025 AT 09:52just read this and i think i’ve been doing it wrong for like 2 years… i used the adult hydrocortisone on my 18mo because it was ‘the same’ and i thought a little dab was fine… turns out i was using like 4x the ftu and on 25% of his body… oh god.
my kid’s fine tho? i think? he didn’t die? maybe? i’m gonna call the dr tomorrow.
also i didn’t know what a ftu was until now. i thought it was a typo for ‘fingertip unit’ but i guess it is. i’m so sorry. i’m a bad parent.
gonna lock the cream up tonight. promise.
rob lafata
December 6, 2025 AT 10:30And you? You’re the one who just said ‘I didn’t know what a FTU was.’
So why are you still using adult cream?
Go buy the pediatric one. Now.
And don’t come back here until you’ve locked it up.
And no - your kid being ‘fine’ doesn’t mean you didn’t risk him. It just means you got lucky.
Again. You’re not a healer. You’re a liability.