Most people assume that when they switch from a brand-name drug to a generic, they’re getting the exact same medicine-just cheaper. And for the most part, that’s true. The active ingredient, the part that actually treats your condition, is identical. But here’s something most patients never think about: inactive ingredients can be totally different. And for some people, those differences matter more than they should.
What Are Inactive Ingredients, Really?
Inactive ingredients, also called excipients, are the stuff in your pill that isn’t the medicine. Think of them as the packaging, the glue, the flavoring, and the filler. They help the pill hold its shape, dissolve at the right time, taste less awful, or stay stable on the shelf. But here’s the catch: they make up most of the pill. In some cases, over 90% of what you swallow isn’t the drug at all. A 2019 MIT study found that nearly every medication contains at least one ingredient that could trigger a reaction in someone with a sensitivity-lactose, gluten, dyes, peanut oil, or FODMAP sugars like lactulose and sorbitol.These ingredients are legal. They’re approved by the FDA. But they’re not required to be clearly labeled as allergens. If your pill has peanut oil, it has to say so. But if it has lactose, gluten, or a dye linked to skin rashes? You’re on your own to find out.
Why Does This Even Matter?
If you’re healthy and don’t have food allergies, you probably won’t notice a difference. But for people with celiac disease, lactose intolerance, asthma, or severe allergies, switching to a generic can mean new symptoms. One patient on Reddit reported severe stomach cramps after switching to generic levothyroxine. The symptoms vanished when she went back to Synthroid. Her pharmacist later confirmed the generic version used lactose as a filler-something the brand-name didn’t.It’s not just digestive issues. People with asthma have reported breathing problems after switching to generics containing sodium metabisulfite, a common preservative. Others get rashes from FD&C red dye or headaches from artificial flavors. These aren’t rare. A MedShadow survey found that 27% of people who switched to generics reported new side effects-and 68% of them blamed the inactive ingredients.
Generic vs Brand: The Real Difference
The FDA requires generics to be bioequivalent to the brand-name drug. That means the active ingredient must be absorbed into your bloodstream at nearly the same rate and amount. The law allows up to 20% variation, but in practice, most generics are within 4%-so the medicine works the same.But there’s no rule for inactive ingredients. Two different generic versions of the same drug can have completely different fillers, coatings, or dyes. One might use corn starch. Another might use wheat starch. One might be coated with a sugar shell. Another might use a dye that triggers migraines in sensitive people. The pill looks the same. The name on the bottle is the same. But inside? Totally different.
And here’s the kicker: even the brand-name drug can change its inactive ingredients over time. Manufacturers update formulations all the time to cut costs or improve stability. So even if you’ve been on the same brand for years, your pill today might not be the same as the one you took five years ago.
Who’s at Risk?
You’re more likely to be affected if you:- Have celiac disease or gluten sensitivity
- Are lactose intolerant
- Have asthma or sulfite sensitivity
- Get rashes or hives from food dyes
- Have irritable bowel syndrome (IBS) and are sensitive to FODMAP sugars
- Take five or more medications daily (polypharmacy)
- Are over 65 (most seniors take multiple drugs, increasing cumulative exposure)
People with multiple conditions are especially vulnerable. Imagine someone with diabetes, high blood pressure, and arthritis-all on generics. Each pill might contain a different sugar, dye, or preservative. Over time, those ingredients add up. One might be harmless alone, but together? They could be enough to trigger fatigue, bloating, or even a flare-up of an autoimmune condition.
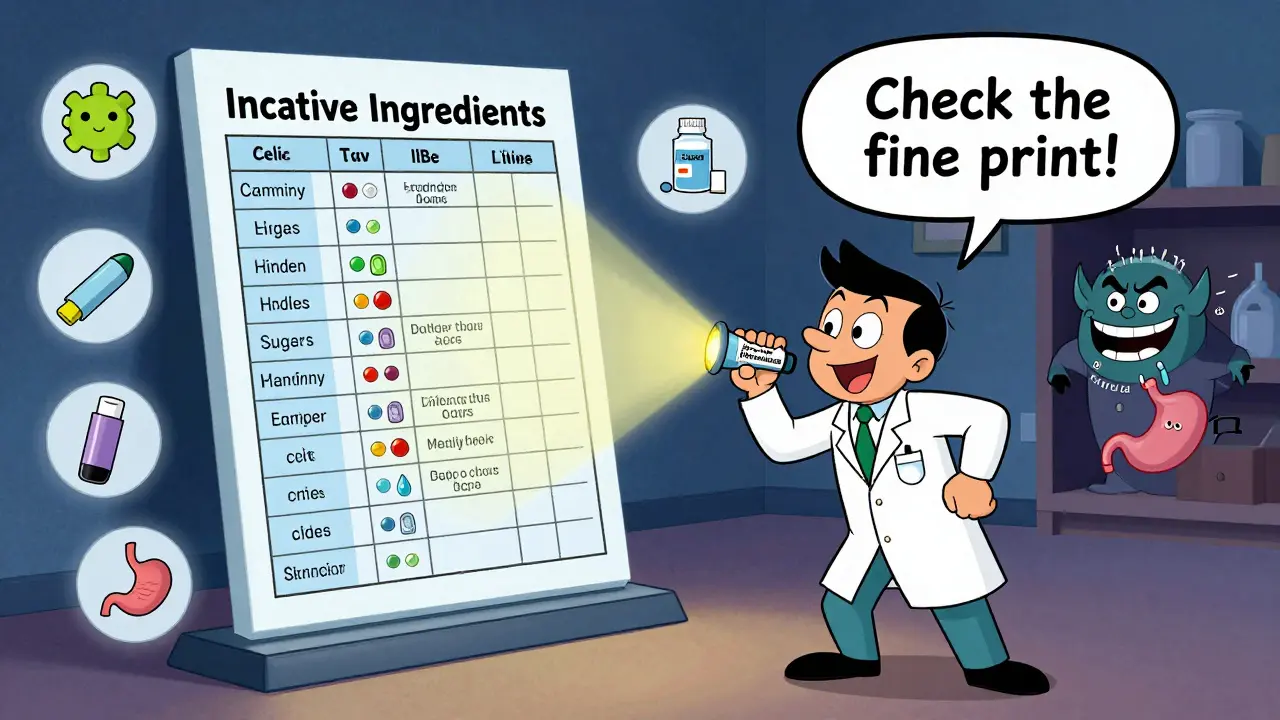
What You Can Do
You don’t have to guess. Here’s how to protect yourself:- Check the label. Look for the “Inactive Ingredients” section on the drug facts panel. It’s usually printed on the box or in the patient information leaflet. If you can’t find it, ask your pharmacist.
- Know your triggers. If you’re allergic to gluten, lactose, or sulfites, write them down. Bring this list to every doctor and pharmacist visit.
- Ask for the manufacturer. Not all generics are made the same. Some companies specialize in allergen-free formulations. Your pharmacist can tell you which manufacturer makes the version you’re getting.
- Don’t switch blindly. If you’re stable on a brand-name drug and you start feeling off after switching to generic, don’t assume it’s “all in your head.” Talk to your doctor. Ask if the inactive ingredients changed.
- Use the FDA’s Inactive Ingredient Database. It’s not user-friendly, but it lists every inactive ingredient approved for use in U.S. medications. Search by drug name to see what’s allowed. It won’t tell you what’s in your specific pill, but it helps you ask better questions.
When to Stick With Brand-Name
There’s no shame in staying on a brand-name drug if it works for you. The FDA says generics are safe and effective for most people. But if you’ve had repeated reactions to generics-or if you have a complex medical history-your doctor can write “Dispense as Written” or “Do Not Substitute” on your prescription. That means the pharmacy can’t switch you without your consent.Some medications are especially sensitive to formulation changes. Levothyroxine (for thyroid), warfarin (a blood thinner), and certain epilepsy drugs have tight therapeutic windows. Even tiny shifts in absorption can cause problems. For these, many doctors recommend sticking with one version-brand or generic-as long as it’s consistent.
What’s Changing?
There’s growing pressure to fix this. Researchers at MIT are building a public database to track inactive ingredients by drug and manufacturer. Patient advocacy groups are pushing for standardized labeling-like nutrition facts for pills. Some generic manufacturers are already responding. A few now offer “hypoallergenic” versions without dyes, gluten, or lactose-though they cost a bit more.For now, the system still favors cost over clarity. But awareness is rising. More pharmacists are trained to ask about sensitivities. More doctors are checking for reactions after switching. And more patients are speaking up.
Bottom Line
Generic drugs save billions of dollars every year. They’re safe for most people. But they’re not magic. The pills you take are complex products, and the parts you can’t see-those fillers, dyes, and preservatives-can have real effects. If you’ve ever felt off after switching to a generic, you’re not imagining it. Ask questions. Demand transparency. Your body knows the difference.Are generic medications less safe than brand-name drugs?
No, generic medications are not less safe. The FDA requires them to meet the same quality, strength, purity, and stability standards as brand-name drugs. The active ingredient is identical, and bioequivalence is strictly tested. However, the inactive ingredients can differ, and those may cause reactions in sensitive individuals. The risk isn’t from the drug’s effectiveness-it’s from the fillers and additives.
Can inactive ingredients in generics cause allergic reactions?
Yes. While rare, inactive ingredients like lactose, gluten, sulfites, and artificial dyes can trigger allergic or intolerance reactions. People with celiac disease, lactose intolerance, asthma, or dye sensitivities are at higher risk. Symptoms can include bloating, rashes, headaches, or breathing difficulties. These reactions aren’t caused by the medicine itself, but by the non-active components in the pill.
How do I find out what’s in my generic medication?
Check the patient information leaflet inside the medication box. Look for a section titled “Inactive Ingredients.” If it’s not there, ask your pharmacist for the manufacturer’s product insert. You can also search the FDA’s Inactive Ingredient Database by drug name to see what ingredients are approved for that medication. But remember: the database doesn’t tell you what’s in your specific bottle-only what’s allowed.
Should I avoid generic medications if I have food allergies?
You don’t need to avoid generics entirely, but you should be cautious. If you’re allergic to gluten, lactose, or other common fillers, always check the inactive ingredients before switching. Ask your pharmacist to compare your current brand with the generic version. Some manufacturers make allergen-free generics-these are often listed as “free-from” options. If you’re unsure, stick with the brand you know works.
Can I ask my doctor to prescribe only brand-name drugs?
Yes. Your doctor can write “Dispense as Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from switching you to a generic without your consent. This is especially important if you’ve had reactions to generics in the past or are taking medications with narrow therapeutic windows, like levothyroxine or warfarin.
Why don’t drug labels clearly warn about allergens like food does?
Current FDA rules only require allergen labeling for ingredients that are major food allergens (like peanuts) and sulfites. Gluten, lactose, and other common triggers aren’t classified as allergens under food labeling laws, so they don’t need to be highlighted. This creates a dangerous gap-patients with celiac or lactose intolerance often don’t realize their medicine contains these ingredients until they react.





Catherine Scutt
January 8, 2026 AT 23:56Ugh, I switched generics last month and got a rash that lasted two weeks. Turned out it was the red dye. No one told me. Why is this even a thing?
Darren McGuff
January 9, 2026 AT 11:58As a pharmacist with 18 years in community practice, I can tell you this is one of the most under-discussed issues in med safety. I’ve had patients come in with unexplained GI flares after switching levothyroxine generics-lactose is the usual culprit. We don’t screen for it because it’s not legally required to be flagged. I keep a printed list of allergen-free generic manufacturers on my desk. Ask your pharmacist for the manufacturer code-it’s the only way to know what’s really in that pill.
Alicia Hasö
January 11, 2026 AT 07:02If you’re someone who takes five or more meds daily, this isn’t just a ‘maybe’ issue-it’s a silent accumulation problem. Think of it like secondhand smoke from your own medicine cabinet. Each pill adds a little more chemical noise. I’ve worked with elderly patients whose fatigue and brain fog cleared after we switched to gluten-free, dye-free generics. It’s not placebo. It’s pharmacology. You deserve to know what’s in your body. Don’t let cost silence your health.
Aron Veldhuizen
January 11, 2026 AT 20:45Let’s be philosophical here: if a pill contains 90% filler, and that filler triggers a reaction, is the drug even the cause of the illness-or is the system itself the pathology? We’ve reduced human biology to a cost-per-dose equation. The FDA approves ingredients based on statistical averages, not individual biochemistry. So we’re not just taking medicine-we’re participating in a grand experiment where you’re the control group that got ignored. The real question isn’t ‘what’s in the pill?’ It’s ‘why do we accept this?’
Ian Long
January 13, 2026 AT 08:45I used to think this was just hypochondria until my mom developed chronic hives after switching to a generic blood pressure med. We traced it to FD&C Yellow No. 6. She’s 72, on six meds. Each one had a different dye. We switched to one brand that offers dye-free versions-cost went up $12/month. Her skin cleared in 48 hours. This isn’t about being ‘difficult.’ It’s about being informed. If your doctor doesn’t know this, ask them to read the FDA’s inactive ingredient database. It’s free.
Patty Walters
January 15, 2026 AT 07:29ps. if u have celiac and take a generic thyroid med… check the fillers. i lost 15 lbs before i realized it was the lactose. my pharmacist was like ‘oh yeah, that one’s bad’ like it was common knowledge. it’s not. ask for the insert. seriously.
Phil Kemling
January 15, 2026 AT 15:46There’s a deeper irony here: we trust pills to be precise, but we accept that their non-active components are treated like background noise. We’ve built a medical system that quantifies efficacy down to the nanogram, yet ignores the molecular weight of discomfort. The body doesn’t care about FDA bioequivalence standards-it only cares if it can digest, absorb, or tolerate what’s inside. Maybe the real failure isn’t the generic-it’s our assumption that biology can be standardized like a factory line.
Jenci Spradlin
January 17, 2026 AT 10:39my aunt had migraines for 6 months after switching to generic metoprolol. turned out it was the artificial flavor. she switched back and poof-gone. pharmacist said ‘most people don’t notice’ but guess what-she did. always ask for the insert. it’s right there on the box, buried under the barcode.
Maggie Noe
January 18, 2026 AT 11:46THIS. IS. REAL. 🙏 I had a panic attack after switching to a generic ibuprofen. Turns out it had sodium metabisulfite. My asthma nurse said it’s in 40% of generics. I now have a printed list of ‘safe’ generics. I keep it in my wallet. If you’re sensitive to anything, DO THIS. Your life might depend on it. 💊🚫
Ashley Kronenwetter
January 20, 2026 AT 00:20While the FDA’s current regulatory framework prioritizes cost-efficiency and bioequivalence, the absence of mandatory allergen labeling for excipients represents a significant gap in patient safety protocols. It is incumbent upon prescribers and pharmacists to proactively disclose formulation changes, particularly for patients with known sensitivities. The onus should not rest solely on the patient to decipher pharmaceutical packaging.
Heather Wilson
January 21, 2026 AT 08:17Let’s be honest-this is just another way the pharmaceutical industry profits off of people’s ignorance. They make generics cheaper by using cheap fillers, then charge more for the ‘hypoallergenic’ versions. Meanwhile, patients with chronic conditions get sicker because they can’t afford to stick with brand-name. It’s capitalism disguised as healthcare. And yes, your ‘quiet’ reaction? It’s not all in your head. It’s in the starch.
Jeffrey Hu
January 21, 2026 AT 11:59Actually, you’re all missing the point. The real issue isn’t the inactive ingredients-it’s that we’ve been conditioned to believe pills are ‘just medicine.’ But they’re not. They’re engineered products, like cereal bars with hidden sugars. The FDA doesn’t regulate fillers because they’re not ‘active’-but ‘active’ doesn’t mean ‘harmless.’ If you’re allergic to peanuts, you don’t eat them, even if they’re not the main ingredient. Same logic applies here. Stop treating pills like magic bullets and start treating them like complex chemical formulations. Which they are.
Elisha Muwanga
January 22, 2026 AT 17:55As an American taxpayer who funds the FDA, I find it unacceptable that our regulatory body allows potentially harmful substances to be hidden in medications under the guise of ‘inactive.’ We demand transparency in food labeling, yet allow pharmaceutical companies to bury allergens in fine print. This isn’t just negligence-it’s institutionalized disregard for patient autonomy. Congress needs to act. Now.