When you’re managing heart disease, it’s common to take several medications at once. Maybe it’s a beta blocker for your blood pressure, a statin for cholesterol, a diuretic to reduce swelling, and an anticoagulant to prevent clots. Sounds straightforward-until you realize that combining multiple heart medications can be dangerous if you don’t know what you’re mixing.
One in four adults over 65 takes five or more prescription drugs. For people with heart conditions, that number is even higher. And here’s the scary part: if you’re on seven or more medications, you have an 82% chance of experiencing a dangerous drug interaction. That’s not a guess. It’s from a major study in Circulation that tracked real patients over years. These aren’t rare side effects. They’re predictable, preventable, and happening far too often.
Why Heart Medications Are Especially Risky
Heart drugs work in delicate balance. They affect your blood pressure, heart rhythm, kidney function, and how your body breaks down other substances. When you add another drug-whether it’s a prescription, an over-the-counter pill, or even a supplement-you’re throwing off that balance.
Take statins, for example. These are among the most commonly prescribed heart medications. They lower cholesterol and reduce heart attack risk. But if you drink grapefruit juice-just one quart a day-you’re putting yourself at serious risk. Grapefruit blocks an enzyme in your gut called CYP3A4, which normally helps break down statins. Without it, the drug builds up in your bloodstream. Levels can spike by 47%. That’s enough to cause rhabdomyolysis, a condition where muscle tissue breaks down and floods your kidneys with toxins. It can lead to kidney failure. And no, it’s not just a few sips. Even a single glass daily can trigger this reaction.
Unsafe Combinations You Need to Avoid
Some combinations are so dangerous they’re listed in FDA safety alerts. Here are the top ones you need to know:
- Statin + Grapefruit Juice: As mentioned, this can cause life-threatening muscle damage. No amount of grapefruit juice is truly safe if you’re on a statin. Orange juice? Fine. Grapefruit? Avoid it completely.
- St. John’s Wort + Beta Blockers or Statins: This popular herbal supplement for mood swings speeds up how fast your liver clears out heart medications. The result? Your blood pressure or cholesterol drops below therapeutic levels. You think your meds are working-until you have a heart event.
- Black Licorice + Blood Pressure Medications: Natural black licorice contains glycyrrhizin, which acts like a mineralocorticoid. It causes your body to hold onto sodium and water, raising blood pressure. If you’re on a calcium channel blocker or beta blocker, this can undo all the work your meds are doing. One candy bar a day is enough to cause problems.
- NSAIDs (Ibuprofen, Naproxen) + Blood Pressure Meds or Anticoagulants: These common painkillers reduce the effectiveness of ACE inhibitors and beta blockers. They also increase bleeding risk when taken with warfarin or apixaban. People often take them for arthritis or back pain without realizing the danger.
- Antihistamines (Diphenhydramine) + QT-Prolonging Drugs: Many sleep aids and cold medicines contain diphenhydramine. In people taking certain heart rhythm drugs like amiodarone or sotalol, this can trigger a dangerous irregular heartbeat called torsades de pointes. It can be fatal.
- Alcohol + Any Heart Medication: Alcohol doesn’t just add calories. It directly interferes with how your liver processes drugs. It can spike blood pressure, slow heart rate too much, or make you dizzy and fall. The National Institute on Alcohol Abuse and Alcoholism says alcohol interacts with over 150 medications-many of them for heart conditions.
- MAO Inhibitors (Antidepressants) + Aged Cheese, Cured Meats, Chocolate: These antidepressants are sometimes used for heart patients with depression. But combining them with tyramine-rich foods can cause a sudden, deadly spike in blood pressure. Even a small bite of blue cheese or a slice of salami can trigger a hypertensive crisis.
What Seems Safe But Isn’t
Many people assume that because something is natural or sold over the counter, it’s harmless. That’s a deadly myth.
Turmeric supplements? They interfere with blood thinners like rivaroxaban and can increase bleeding risk. Coenzyme Q10? It can reduce the effect of warfarin. Magnesium? It can lower blood pressure too much when combined with calcium channel blockers. Even fish oil-often recommended for heart health-can thin your blood and increase bleeding when taken with aspirin or clopidogrel.
And don’t forget antacids. If you take omeprazole or famotidine for heartburn, they can change how your body absorbs other drugs. Some cardiac meds need an empty stomach. Others need food. Mixing them up reduces effectiveness. One study showed that taking a calcium channel blocker with an antacid reduced its absorption by up to 40%.

How to Stay Safe
Knowledge is your best defense. Here’s what actually works:
- Use One Pharmacy: All your prescriptions-every single one-should come from the same pharmacy. That way, their system can cross-check every new script against everything else you’re taking. Most chain pharmacies have automated interaction alerts. But if you use multiple pharmacies, those alerts don’t work.
- Do a Brown Bag Review: Every six months, take every pill, capsule, and bottle you take-prescription, OTC, supplements, herbal remedies-and bring them to your doctor or pharmacist. Don’t just list them. Bring the actual bottles. You’ll be surprised how often you forget something or take the wrong dose.
- Keep an Updated Medication List: Write down every drug, the dose, and why you take it. Update it after every doctor visit. Keep a copy in your wallet and on your phone. If you end up in the ER, this could save your life.
- Ask About Alternatives: If your doctor prescribes a new drug, ask: “Is there a safer option that won’t interact with what I’m already taking?” Sometimes, switching from one statin to another, or from ibuprofen to acetaminophen, eliminates the risk entirely.
- Know Your Genetic Risk: Some people metabolize drugs slower or faster due to genetics. The CYP2C9 and CYP3A4 genes are especially important for heart meds. If you’ve had unexpected side effects or poor response to medications, ask about pharmacogenomic testing. It’s not routine yet-but it’s becoming more accessible.
Who’s at Highest Risk?
It’s not just older adults. It’s older adults with multiple conditions. The highest risk group? People over 65 with heart failure, diabetes, and kidney disease. They’re often on six to ten medications. A study from Jimma University found that 77% of hospitalized heart patients had at least one dangerous drug interaction. That’s nearly four out of five.
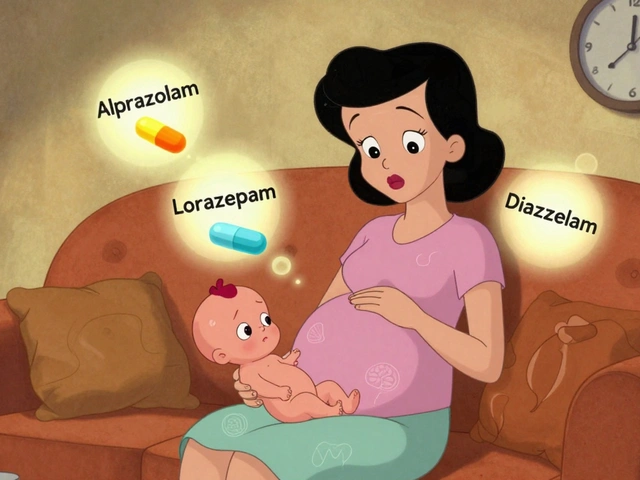
Women are also at higher risk. They tend to take more medications than men and are more likely to be prescribed multiple drugs for overlapping conditions. And because they often weigh less, the same dose can have a stronger effect.
And here’s something no one talks about: depression. People with heart disease are twice as likely to be depressed. Many are prescribed antidepressants. But mixing those with heart meds? That’s a minefield. MAO inhibitors are especially risky, but even SSRIs like sertraline can interact with statins and antiarrhythmics.
What to Do If You Think You’ve Had an Interaction
Symptoms of a bad drug interaction include:
- Sudden dizziness or fainting
- Unexplained muscle pain or weakness
- Swelling in your legs or ankles
- Unusual bruising or bleeding
- Heart palpitations or skipped beats
- Severe fatigue or confusion
If you experience any of these after starting a new medication or changing your routine, don’t wait. Call your doctor or pharmacist immediately. Don’t stop your meds on your own-but don’t keep taking them either without advice.
What’s Changing in 2026
Technology is catching up. Electronic health records now flag potential interactions, but they still miss about 23% of dangerous combinations. Why? Because they don’t always know what supplements you’re taking, or whether you’ve skipped a dose, or if you’ve been drinking grapefruit juice.
Researchers are now testing AI tools that look at your full medical history, genetic profile, and even your pharmacy refill patterns to predict interactions before they happen. Some hospitals in Canada and the U.S. are already using these systems for high-risk patients.
But until those tools are universal, you’re still your own best protector. The more you know about what you’re taking-and why-you can avoid becoming a statistic.
Can I take ibuprofen if I’m on a blood pressure medication?
It’s risky. Ibuprofen and other NSAIDs can reduce the effectiveness of ACE inhibitors, beta blockers, and diuretics. They can also raise your blood pressure and increase your risk of kidney damage, especially if you already have heart or kidney issues. Acetaminophen (Tylenol) is usually a safer choice for pain relief, but always check with your doctor first.
Is it safe to drink alcohol with heart meds?
Not really. Alcohol can worsen heart rhythm problems, lower blood pressure too much, and interfere with how your liver processes medications. It can make you dizzy, increase your risk of falls, and reduce the effectiveness of drugs like beta blockers and anticoagulants. If you drink, talk to your doctor about how much-if any-is safe for you.
Can I stop taking a medication if I think it’s causing side effects?
Never stop a heart medication on your own. Even if you think it’s causing a problem, stopping suddenly can trigger a heart attack, stroke, or dangerous rebound in blood pressure. Call your doctor instead. They can help you adjust safely or switch to a different drug.
Do supplements like CoQ10 or magnesium help with heart meds?
Some people take them hoping to reduce side effects, like muscle pain from statins. But supplements aren’t regulated like drugs. CoQ10 can reduce the effect of warfarin. Magnesium can lower blood pressure too much when combined with calcium channel blockers. Always tell your doctor what you’re taking-even if you think it’s harmless.
How do I know if my pharmacy is checking for drug interactions?
If you get all your prescriptions filled at one pharmacy, they should be checking automatically. But if you’re unsure, ask your pharmacist directly: “Do you screen all my medications for interactions?” If they say yes, ask them to show you the list of drugs they checked. If they don’t, it’s time to switch pharmacies.
What should I do if I’m prescribed a new medication?
Before you fill the script, ask three questions: 1) What is this for? 2) How does it interact with what I’m already taking? 3) Is there a safer alternative? Write down the answers. Don’t rely on memory. Many dangerous interactions happen because patients assume the doctor already checked everything.
Final Thought
Heart medications save lives. But they’re not harmless. The more you take, the more you need to be vigilant. It’s not about being scared-it’s about being smart. A single conversation with your pharmacist, a simple brown bag review, or just avoiding grapefruit juice could prevent a hospital stay-or worse.
You’re not alone in this. Millions of people manage complex heart medication regimens every day. But only those who ask questions, keep track, and speak up stay safe.




Susan Arlene
January 5, 2026 AT 21:48Joann Absi
January 6, 2026 AT 20:18Mukesh Pareek
January 8, 2026 AT 13:02Ashley S
January 9, 2026 AT 14:19Jeane Hendrix
January 9, 2026 AT 14:21Rachel Wermager
January 11, 2026 AT 04:17Tom Swinton
January 11, 2026 AT 11:03Leonard Shit
January 11, 2026 AT 18:13Wesley Pereira
January 12, 2026 AT 04:31Isaac Jules
January 13, 2026 AT 01:07Amy Le
January 14, 2026 AT 15:28Pavan Vora
January 15, 2026 AT 01:37Stuart Shield
January 15, 2026 AT 05:35