Ethinylestradiol, a synthetic version of estrogen, is a key ingredient in many contraceptive pills and hormone replacement therapies. Its interaction with the skin can be both beneficial and problematic.
In this article, we'll dive into what ethinylestradiol is, investigate its impact on acne, explore its positive effects on skin, and share practical tips for managing skin health while using this hormone. Whether you're looking to better understand your contraceptive's side effects or hoping for clearer skin, this guide aims to shed some light.
- What is Ethinylestradiol?
- Ethinylestradiol and Acne
- Positive Effects on Skin
- Tips for Healthy Skin Management
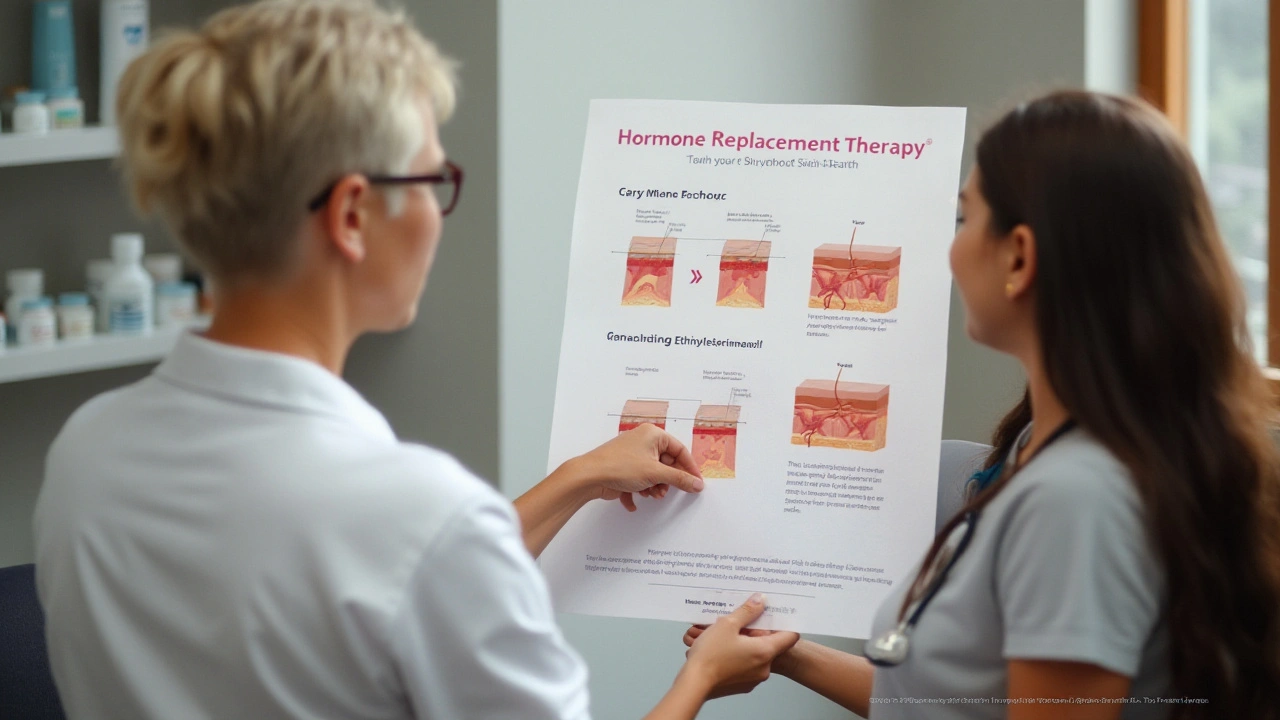
What is Ethinylestradiol?
Ethinylestradiol is a synthetic form of estrogen, a hormone that's naturally produced in the human body. Estrogen plays a critical role in regulating various bodily functions, ranging from reproductive health to maintaining skin and hair. Ethinylestradiol is commonly found in birth control pills and hormone replacement therapy (HRT), making it one of the most widely studied synthetic hormones.
Originally developed in the mid-20th century, ethinylestradiol was created to be more effective and longer-lasting than natural estrogens. Its primary use is to prevent ovulation, thereby preventing pregnancy. But aside from its contraceptive properties, it also has significant effects on the skin. Many users notice changes in their skin health, which can be either positive or negative.
The molecular structure of ethinylestradiol enables it to bind effectively to estrogen receptors in the body. This property makes it potent, ensuring that even low doses can exert considerable effects. This binding influences the skin by regulating sebum production, affecting the growth cycle of skin cells, and modulating the immune responses in the skin.
According to Dr. Susan Hu, a dermatologist specializing in hormonal skin conditions, "Ethinylestradiol can both alleviate and exacerbate skin issues depending on the individual's unique hormonal environment and skin type."
One of the most well-known effects of ethinylestradiol is its impact on acne. This hormone reduces the levels of free testosterone in the bloodstream, which in turn decreases the production of sebum, an oily substance that can clog pores and cause acne. It's no wonder, then, that many dermatologists prescribe birth control pills containing ethinylestradiol to women suffering from hormonal acne.
Despite these benefits, ethinylestradiol isn't without its drawbacks. For some women, the hormone can cause hyperpigmentation, commonly known as melasma, where dark patches appear on the skin. This side effect can be particularly distressing and may take months or even years to fade. Additionally, some may experience increased redness or rosacea as blood vessels in the skin become more responsive to the hormone.
Ethinylestradiol's impact extends beyond just acne and pigmentation. The hormone can also influence the skin's overall texture and moisture levels. Some women report improved elasticity and hydration, while others may find their skin becomes dry and flaky. Understanding these effects requires a personalized approach, as the hormone's interaction with each person's skin biology can vary significantly.
Given its wide-ranging effects, it's essential to consult healthcare professionals for advice tailored to your specific needs before starting any medication containing ethinylestradiol. Being well-informed about how this hormone interacts with your skin can help you make more educated choices regarding your hormonal therapy or contraceptive options.
Ethinylestradiol and Acne
Ethinylestradiol, a commonly used synthetic estrogen in many contraceptive pills, is known to have a significant impact on acne. Acne is a skin condition that arises when hair follicles become clogged with oil and dead skin cells. Hormonal fluctuations can trigger an increase in sebum production, which plays a big role in acne formation.
When it comes to ethinylestradiol's effect on the skin, it has been found to have both positive and negative outcomes. One of the ways this hormone helps to combat acne is by reducing the levels of androgens, male hormones that can increase sebum production. Reduced sebum can result in fewer and less severe acne breakouts.
Additionally, ethinylestradiol-containing contraceptives have been approved by the FDA specifically for the treatment of acne in women. These contraceptives work by balancing the hormonal fluctuations that often lead to acne. A 2012 study published in the “Journal of the American Academy of Dermatology” revealed that oral contraceptives containing ethinylestradiol can be effective in improving acne in women, making it a popular choice for many facing skin issues triggered by hormonal imbalance.
However, it is crucial to note that not everyone responds to ethinylestradiol in the same way. For some women, the introduction of synthetic estrogen can initially cause a flare-up in acne before improvement is seen. This initial reaction can be attributed to the body's process of adjusting to new hormonal levels. Patience and continuity in using the medication are often advised to see the full benefit.
“Oral contraceptives containing ethinylestradiol can be particularly effective against hormonal acne, reducing symptoms significantly after the adjustment period,” states Dr. Jennifer Gordon, a board-certified dermatologist.
While ethinylestradiol may work wonders for some, others might experience side effects such as increased sensitivity or allergic reactions, which can lead to skin issues. Consulting a healthcare professional for a personalized approach is essential before starting any new hormonal treatment.
For those experiencing acne while on ethinylestradiol, integrating a supportive skincare routine can aid in managing symptoms. Gentle, non-comedogenic products can help maintain a healthy balance of oils in the skin. Additionally, staying well-hydrated and maintaining a balanced diet are excellent practices that contribute to overall skin health.
Understanding how ethinylestradiol interacts with the skin helps to demystify its effects and allows for better management of acne and other skin conditions. By acknowledging the hormone's potential benefits and drawbacks, women can make informed choices about their skincare and contraception options.

Positive Effects on Skin
When it comes to the positive impacts of ethinylestradiol on skin health, there are several noteworthy benefits. For those who've been battling acne, ethinylestradiol can be a game changer. This synthetic estrogen helps to regulate hormonal fluctuations that often lead to breakouts. By stabilizing these hormones, ethinylestradiol can reduce both the frequency and severity of acne outbreaks.
Now, let's talk about skin texture and elasticity. Estrogen, including its synthetic form, plays a crucial role in the production of collagen and elastin, which are essential proteins for maintaining firm and youthful skin. As we age, natural estrogen levels decline, leading to a loss of skin elasticity and the appearance of wrinkles. Ethinylestradiol can help slow this process by promoting healthy skin structure and hydration.
Studies have shown that users of ethinylestradiol-based hormonal therapies often report a noticeable improvement in skin radiance and smoothness. This is partly because estrogen enhances blood flow to the skin, providing vital nutrients and oxygen that keep the skin looking vibrant and youthful.

Tips for Healthy Skin Management
Managing your skin health while using ethinylestradiol can be a bit of a balancing act, but it’s entirely achievable with the right strategies. First and foremost, maintain a consistent skincare routine tailored to your skin type. Cleansing, moisturizing, and using sunscreen are the foundational steps you shouldn't skip. The interplay between this synthetic hormone and your skin can sometimes lead to side effects like dryness or even excessive oil production. Keeping your routine straightforward but effective is key.
Another vital tip is to stay hydrated. Drinking plenty of water helps keep your skin supple and youthful. Ethinylestradiol has been noted to cause water retention, but that shouldn't deter you from your daily intake of 8 glasses of water. Proper hydration supports your skin's barrier function and promotes detoxification, which is essential for combating acne and dullness.
It's also important to be mindful of your diet. Eating a balanced diet rich in antioxidants, like fruits and vegetables, can significantly improve your skin's texture and overall appearance. Nutrients such as vitamins A, C, and E are known to support skin health. Omega-3 fatty acids found in fish and flaxseeds are also excellent for reducing inflammation and keeping your skin moisturized. A healthy inside often reflects a glowing outside.
Don’t underestimate the power of sleep. Adequate rest allows your skin to undergo repair and regeneration processes. Aim for at least 7-8 hours of sleep per night. Incorporating a nighttime skincare routine that includes hydrating serums or treatments can enhance your skin's natural rejuvenation cycle.
Stress management is another crucial aspect. Stress can exacerbate skin conditions like acne. Practices such as yoga, meditation, or simple deep-breathing exercises can make a significant difference. Learn what calms you and make it a regular part of your routine.
Avoid Over-Exfoliating
While it might be tempting to scrub away imperfections, over-exfoliating can strip your skin of its natural oils, leading to irritation and increased sensitivity. Stick to exfoliating once or twice a week and opt for gentle exfoliants. This moderation helps maintain the skin's natural barrier while still removing dead skin cells.
Consulting with a dermatologist can provide personalized advice and treatment options tailored to your skin's needs. If you're noticing any adverse effects like severe acne or rashes, it's worth seeking professional guidance. Dermatologists can recommend specialized skincare products or treatments that align with your skin's unique characteristics.
"Prevention is the key. Keep your routine simple but consistent, and always listen to your skin's needs." — Dr. Jane Smith, Dermatologist
Above all, patience is your ally when it comes to achieving healthy skin while using ethinylestradiol. It may take some time to find the perfect balance in your routine and lifestyle. But with diligence and the right approach, you can enjoy the benefits of this hormone without compromising your skin health.




Karla Luis
September 20, 2024 AT 15:32jon sanctus
September 21, 2024 AT 11:48Kenneth Narvaez
September 22, 2024 AT 07:37Christian Mutti
September 23, 2024 AT 16:58Liliana Lawrence
September 23, 2024 AT 22:08Sharmita Datta
September 24, 2024 AT 19:29mona gabriel
September 25, 2024 AT 18:09Phillip Gerringer
September 25, 2024 AT 18:47jeff melvin
September 26, 2024 AT 02:15Matt Webster
September 27, 2024 AT 23:00Stephen Wark
September 29, 2024 AT 20:55Daniel McKnight
September 30, 2024 AT 09:34Jaylen Baker
September 30, 2024 AT 22:21Fiona Hoxhaj
October 2, 2024 AT 08:13Merlin Maria
October 3, 2024 AT 14:24Nagamani Thaviti
October 3, 2024 AT 17:52Hamza Asghar
October 4, 2024 AT 15:07Kamal Virk
October 5, 2024 AT 21:48