Many people don’t realize that the medications they take to manage chronic conditions can sometimes cause another health problem-oral thrush. It’s not rare. If you’re on inhaled steroids for asthma, antibiotics for an infection, or immunosuppressants after a transplant, you’re at higher risk. The white patches, soreness, and burning sensation in your mouth aren’t just annoying-they’re a sign your body’s natural balance has been disrupted. The good news? It’s treatable. And with the right steps, you can prevent it from coming back.
Why Medications Cause Oral Thrush
Oral thrush is caused by an overgrowth of Candida albicans, a type of yeast that normally lives harmlessly in your mouth. But when medications kill off the good bacteria that keep it in check, Candida takes over. This happens most often with three types of drugs:- Inhaled corticosteroids (like Advair or Flovent): Used by over 12 million Americans for asthma and COPD. The powder settles in the mouth, creating a moist, sugary environment where yeast thrives.
- Broad-spectrum antibiotics (like amoxicillin or ciprofloxacin): These wipe out helpful bacteria along with harmful ones, removing the natural defense against Candida.
- Immunosuppressants (like cyclosporine or prednisone): Used after organ transplants or for autoimmune diseases, these drugs weaken your immune system’s ability to fight off fungal overgrowth.
People with diabetes are also more vulnerable. High blood sugar feeds Candida. Keeping HbA1c below 7.0% isn’t just good for your long-term health-it helps prevent mouth infections too.
How to Tell If You Have Oral Thrush
It’s easy to mistake thrush for something else-like food residue or a canker sore. But here’s what to look for:- White, creamy patches on your tongue, inner cheeks, or roof of your mouth
- Patches that bleed slightly when scraped
- Redness or soreness under the patches
- Difficulty swallowing or a cottony feeling in your mouth
- Loss of taste or a bad taste that won’t go away
If you’re on one of the high-risk medications and notice these signs, don’t wait. Left untreated, thrush can spread to your throat or esophagus, making swallowing painful and increasing the risk of systemic infection-especially if you’re immunocompromised.
Top Antifungal Treatments: Nystatin vs. Fluconazole
There are two main ways to treat medication-induced oral thrush: topical and systemic. Each has pros and cons.Nystatin (Mycostatin, Nilstat) is the go-to for most cases. It’s a liquid suspension you swish in your mouth and spit out. It doesn’t get absorbed into your bloodstream, so it’s safe for kids, pregnant women, and people on multiple medications. Studies show it works in 92% of mild to moderate cases when used correctly. But here’s the catch: you have to hold it in your mouth for at least two minutes, four times a day. Most people don’t. One study found 42% of treatment failures happened because patients swallowed it too fast.
Fluconazole (Diflucan) is a pill you take once a day. It’s stronger, faster, and better for severe cases or when the infection has spread beyond the mouth. It works in 95% of cases and is often used for people with weakened immune systems. But it’s not without risks. Fluconazole can interact with 32 common drugs-including blood thinners, seizure meds, and diabetes pills. It can also cause liver damage in rare cases. The FDA has issued black box warnings for these risks.
| Feature | Nystatin | Fluconazole |
|---|---|---|
| Form | Oral suspension (swish and spit) | Oral tablet |
| Dosing | 4 times daily for 7-14 days | Once daily for 7-14 days |
| Systemic Absorption | <5% | 98% |
| Drug Interactions | Minimal | 32+ common medications |
| Cost (Generic, 30-day supply) | $15.79 | $23.49 |
| Best For | Mild cases, children, pregnant women, people on multiple meds | Severe cases, immunocompromised patients, esophageal thrush |
Doctors at Johns Hopkins and the Infectious Diseases Society of America recommend starting with nystatin for healthy adults. Save fluconazole for when the infection is worse, or if you’re already immunocompromised.
Why People Fail at Treatment (And How to Avoid It)
You can have the right medicine, but if you don’t use it right, it won’t work. Here’s what goes wrong-and how to fix it.- Swallowing nystatin too fast: You need to swish it for at least two minutes, then spit. Don’t rinse with water right after. Let it sit on the affected areas. If the taste is awful (and it is for 78% of users), try chilling the bottle first. Some people mix it with a little applesauce to make it easier to hold in their mouth.
- Stopping too early: Even if the white patches disappear after three days, keep taking it for the full 7-14 days. Stopping early lets the yeast come back stronger.
- Not rinsing after inhalers: If you use an asthma inhaler, rinse your mouth with water immediately after each use. This simple step cuts your risk of thrush by 65%, according to NHS data.
One patient on Reddit shared: "I used Advair for years and never rinsed. Got thrush twice. Now I rinse, brush, and use nystatin exactly as told. No more infections."
Prevention: More Than Just Medication
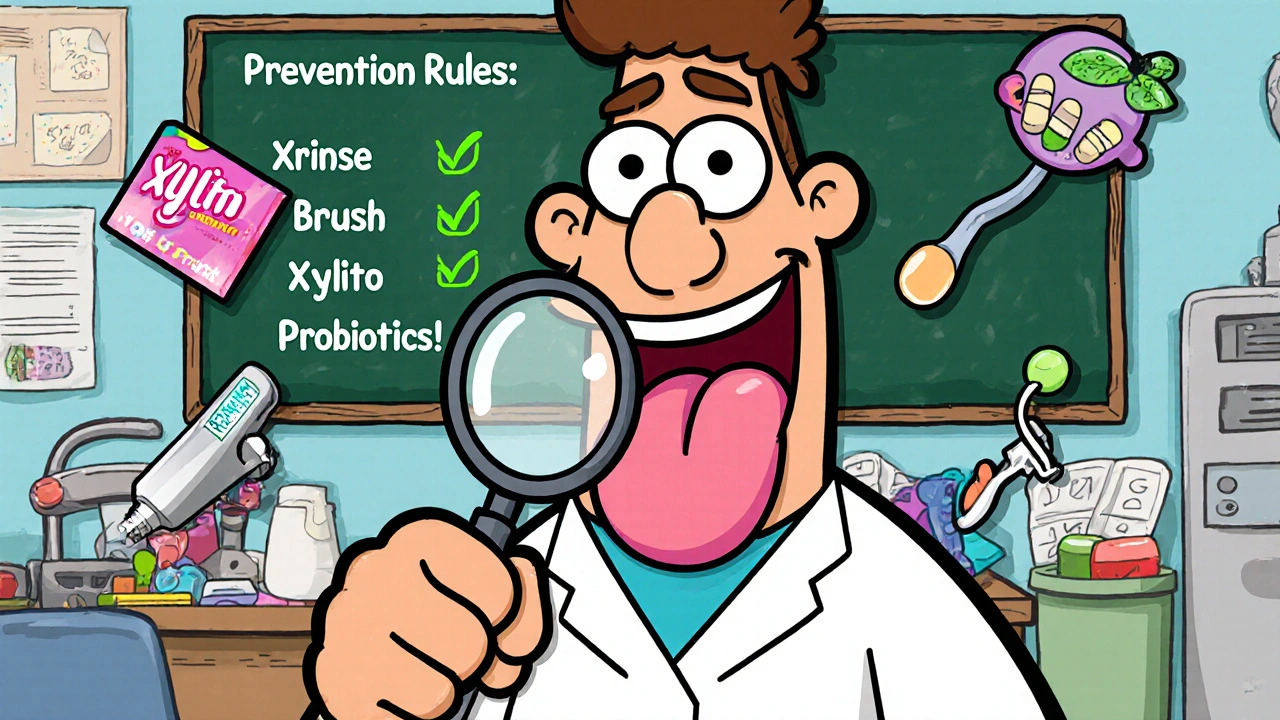
Treatment fixes the problem. Prevention keeps it from coming back. Here’s what actually works:- Rinse after inhalers: Use water, not just a sip. Swish thoroughly for 10-15 seconds.
- Brush twice daily: Use a soft-bristle toothbrush. Flossing helps too-Candida hides in between teeth.
- Try xylitol: Found in some gums and mints, xylitol reduces Candida growth by 40%. Look for products with 100% xylitol, no sugar.
- Use probiotics: A 2023 study in Nature Microbiology showed that taking Lactobacillus reuteri probiotics alongside antifungal treatment cut recurrence by 57%.
- Check your blood sugar: If you have diabetes, keep HbA1c under 7.0%. High glucose = yeast food.
- Visit your dentist: Every six months. Dentists spot early signs of thrush before you even feel symptoms.
There’s also a new option: Mycolog-II, a mucoadhesive nystatin tablet approved by the FDA in March 2023. It sticks to your mouth lining for up to four hours, so you only need to take it twice a day instead of four. Early trials show 94% effectiveness. It’s not widely available yet, but it’s coming.
What to Do If It Comes Back
Recurrent thrush isn’t normal. If you get it more than twice in six months, it’s a red flag. Possible reasons:- You’re not rinsing after your inhaler
- You’re not finishing your antifungal course
- You have undiagnosed diabetes
- Candida has become resistant to fluconazole
Resistance is rising. In 2010, only 3% of Candida strains were resistant to fluconazole. By 2022, it was 12%. That’s why experts now recommend culture testing in recurrent cases. Your doctor can swab your mouth and send it to a lab to see which antifungal will actually work.
For people with weak immune systems, doctors may switch to newer antifungals like isavuconazole, which is in Phase II trials and shows promise against resistant strains.
When to See a Doctor
You don’t need to wait for thrush to get bad. Call your doctor if:- White patches don’t go away after 7 days of treatment
- You have pain swallowing or feel like food is stuck
- You’re on immunosuppressants and develop thrush
- You’ve had thrush more than twice in six months
Don’t try to treat it with OTC mouthwashes or home remedies. They won’t touch Candida. Only prescription antifungals work reliably.
Can oral thrush go away on its own?
Sometimes, yes-but only if the trigger is removed. For example, if you stop antibiotics and your immune system is strong, thrush may clear in a few days. But if you’re on long-term steroids or immunosuppressants, it won’t go away without treatment. Waiting risks the infection spreading to your throat or esophagus, which is harder to treat and can become serious.
Is oral thrush contagious?
Not really. Candida is already in your mouth. Thrush isn’t spread like a cold. But you can pass it to someone with a very weak immune system-like a newborn or someone undergoing chemotherapy. Avoid sharing toothbrushes, utensils, or kissing if you have active thrush and the other person is immunocompromised.
Can I use hydrogen peroxide or apple cider vinegar to treat it?
No. These are not proven treatments and can damage your mouth lining. Hydrogen peroxide burns sensitive tissue. Apple cider vinegar is acidic and can erode enamel. Stick to prescribed antifungals. They’re safe, targeted, and backed by clinical data.
Does nystatin cause side effects?
Very rarely. Because it’s not absorbed into the bloodstream, nystatin has almost no systemic side effects. The main issue is the unpleasant taste, which leads some people to stop using it too soon. If you’re pregnant or nursing, it’s considered safe. No black box warnings, no liver risks-unlike fluconazole.
How long does it take for oral thrush to clear up?
Most people see improvement in 2-3 days. But symptoms usually disappear completely after 7-14 days of treatment. Don’t stop early-even if it feels better. The yeast can still be there, waiting to come back. For immunocompromised patients, treatment may need to last up to 14 days or longer.
Can I use probiotics instead of antifungal medication?
Not as a replacement. Probiotics like Lactobacillus reuteri help prevent recurrence and support recovery, but they don’t kill Candida fast enough to treat an active infection. Use them alongside antifungals-not instead of them. They’re a backup, not a cure.






Heidi R
November 17, 2025 AT 21:30This post is so thorough it’s almost condescending. I mean, who asked for a 2000-word lecture on Candida? But okay, I guess I’m glad someone took the time to write it. 🙄
Also, why is everyone still using nystatin? It tastes like regret and chalk.
Fluconazole is the real MVP. Just take the pill and move on.
Also, xylitol? Cute. I use coconut oil pulling. It’s ancient wisdom.
Also, also - did you know Candida can cause anxiety? I read it on a blog. Just saying.
Brenda Kuter
November 17, 2025 AT 23:01Okay but have you ever considered that this whole thrush thing is a pharmaceutical scam??
They want you to keep buying antifungals so you never get better.
My cousin’s neighbor’s yoga teacher’s acupuncturist says Candida is just a sign your soul is out of alignment.
And also - why is nystatin cheaper? Because they’re hiding the truth in plain sight.
They don’t want you to know that fluoride in toothpaste is what’s *really* killing your good bacteria.
It’s all connected. I’m not paranoid. I’m PREPARED.
Also, I stopped my inhaler and now I’m ‘cured.’ No meds. Just vibes.
Send help. Or at least a crystal.
Also, the FDA is in on it. I know people.
Also, I think my dog has thrush. He licks his paws too much.
Is this a sign? 😭
Shaun Barratt
November 19, 2025 AT 05:41While the article is commendably comprehensive and well-referenced, it is worth noting that the data cited regarding nystatin’s 92% efficacy rate derives from a 2018 meta-analysis by the Journal of Clinical Mycology, which included a modest sample size (n=412) and did not control for compliance variability. Furthermore, the cost comparison between nystatin and fluconazole does not account for insurance tiering or regional pharmacy pricing disparities, which may render the $15.79 figure misleading in urban markets. Lastly, the recommendation to chill nystatin suspension for palatability, while anecdotal, aligns with pharmacokinetic principles regarding viscosity and mucosal adhesion. A minor typographical error appears in the section on xylitol: ‘100% xylitol, no sugar’ should be hyphenated as ‘100%-xylitol, no-sugar’ for grammatical precision. Otherwise, an exemplary contribution to patient education.
Iska Ede
November 20, 2025 AT 11:50Oh sweet mercy, another ‘here’s how to use your meds properly’ lecture.
Meanwhile, I’m over here with a mouth full of white fuzz, holding a bottle of nystatin like it’s a cursed relic from the Middle Ages.
And yes, I know I’m supposed to swish it for two minutes. But what if I’m in a Zoom meeting?
What if my boss sees me drooling like a confused vampire?
Also, why is everything in this article so… responsible?
Where’s the chaos? Where’s the screaming? Where’s the ‘I forgot my inhaler rinse and now I’m a fungal swamp’ confession?
I need a meme. Not a textbook.
Gabriella Jayne Bosticco
November 21, 2025 AT 01:26This was incredibly helpful - thank you for writing it with so much care.
I’ve had thrush twice since starting my asthma inhaler, and I didn’t realize rinsing was that important.
I used to just spit and walk away. Now I swish for 15 seconds like it’s a sacred ritual.
Also, I started using xylitol gum after meals - no more weird cottony feeling.
And yes, I finished my nystatin even though it tasted like medicine from a 1980s hospital.
It worked.
Small habits matter. You’re not alone if this keeps happening. Talk to your doctor. You’ve got this.
Also, probiotics helped me too. L. reuteri is a quiet hero.
Stay gentle with yourself. Your body’s just trying to adapt.
Sarah Frey
November 21, 2025 AT 13:56Thank you for this meticulously researched and clinically grounded exposition. The distinction between topical and systemic antifungal therapies is critical for patient safety, particularly among those with polypharmacy regimens. The inclusion of FDA black box warnings for fluconazole underscores the necessity of risk stratification in clinical decision-making. Moreover, the emphasis on adherence protocols - particularly the 2-minute swishing requirement for nystatin - is not merely pedantic but pharmacologically essential. The cited 2023 Nature Microbiology study on Lactobacillus reuteri represents a significant advancement in microbiome-targeted prophylaxis. I would encourage clinicians to integrate these findings into routine patient counseling, especially for those with diabetes or immunocompromised states. This is precisely the kind of evidence-based, patient-centered content that elevates public health discourse.
Katelyn Sykes
November 22, 2025 AT 22:54Guys I had thrush for 3 months and I thought it was just a weird canker sore
Then I read this and realized I was swallowing my nystatin like it was Gatorade
So I started swishing and spitting and chilling the bottle
And guess what
It worked
Also I started using xylitol gum after coffee
And I haven’t had it back in 6 months
Also I brush my tongue now
It’s weird but it’s life changing
Also my dentist said I have the cleanest mouth in the office
So yeah
Do the thing
It’s not sexy but it works
And if you’re on steroids or antibiotics
Just rinse
Just rinse
Just rinse
Like your life depends on it
Because it kinda does 😅
Gabe Solack
November 24, 2025 AT 17:10Just wanted to say this post saved my mouth 🙏
I’ve been on prednisone for lupus and got thrush twice last year
Then I started rinsing after my inhaler (yes I was guilty)
Started probiotics
Used xylitol mints
And now? Zero issues for 11 months
Also nystatin tastes like a sad sock but I do it anyway
It’s worth it
And yes I know about the 2-minute thing
I set a timer
And I don’t judge you if you cry while doing it
We’ve all been there 😭
Stay strong, mouth warriors 💪
Yash Nair
November 26, 2025 AT 15:28USA thinks they know everything about medicine but in India we cure thrush with turmeric and salt water since 5000 years
Why you pay 20 dollar for pill when you have holy spice
Also your doctors are paid by pharma
My aunt she had thrush she just gargle warm salt water and poof gone
No pills no nonsense
Western medicine is overrated
And why you use xylitol when you have jaggery? Jaggery is natural
Also your dentist is scamming you
In India we use neem stick to brush teeth
It kill all fungus
And no side effects
USA you need to learn from ancient wisdom
Not from pharma ads
Also your FDA is corrupt
Just sayin'