Diphenhydramine Risk Calculator
This tool helps you understand your personal risk when using diphenhydramine (Benadryl, Unisom, ZzzQuil) for sleep.
Your Risk Assessment
Your Risk Assessment
Safer Alternatives
Many people reach for diphenhydramine when they can’t fall asleep-brands like Benadryl, Unisom, or ZzzQuil are easy to grab off the shelf, cheap, and promise quick results. But here’s the truth: what works the first night often stops working by the third, and the next-day fog might stick around longer than the sleep did. If you’ve ever woken up feeling like you ran a marathon in your sleep, only to stumble through your morning coffee with brain fog, you’re not alone. And you’re not safe either-especially if you’re over 65.
How Diphenhydramine Actually Works (And Why It’s Not What You Think)
Diphenhydramine isn’t a sleep drug. It’s an antihistamine, originally designed to treat allergies. Its sleep-inducing effect is a side effect-one that happens because it blocks histamine in the brain. Histamine keeps you alert. Knock it out, and you get drowsy. Simple, right? But here’s the catch: diphenhydramine doesn’t just block histamine. It also messes with acetylcholine, a key brain chemical involved in memory, focus, and muscle control. That’s why you get dry mouth, blurred vision, constipation, and confusion-not just tiredness.
For young, healthy adults, this might feel like a minor trade-off. But for older adults, it’s a different story. Studies show that in people over 65, diphenhydramine can stay in the body nearly twice as long as it does in younger people. That means the drowsiness doesn’t fade by morning-it lingers. And with it comes a higher risk of falls, confusion, and even memory loss.
The Hidden Dangers: More Than Just Grogginess
Most people think the worst side effect is being sleepy the next day. But the real risks are quieter-and far more dangerous.
- Increased dementia risk: A 2024 study from Johns Hopkins tracked over 3,000 adults over 65 for seven years. Those who regularly used diphenhydramine had a 54% higher chance of developing dementia. This isn’t correlation-it’s a direct link tied to how the drug blocks acetylcholine, a neurotransmitter already declining with age.
- Urinary problems: For men over 65 with enlarged prostates, diphenhydramine can make it nearly impossible to urinate. That’s not just uncomfortable-it can lead to hospitalization.
- Confusion and hallucinations: The FDA updated warning labels in 2023 after reports of older adults experiencing hallucinations, paranoia, and severe disorientation after just a few doses.
- Driving danger: One study found that 50 mg of diphenhydramine impaired driving ability as much as a blood alcohol level of 0.10%-well above the legal limit in every U.S. state.
And here’s the kicker: the FDA says diphenhydramine is only meant for occasional sleeplessness-no more than 14 days in a row. But a 2022 study found that 73% of users kept taking it past that limit. Why? Because it seemed to work… at first.
Why It Stops Working (And What Happens When You Keep Using It)
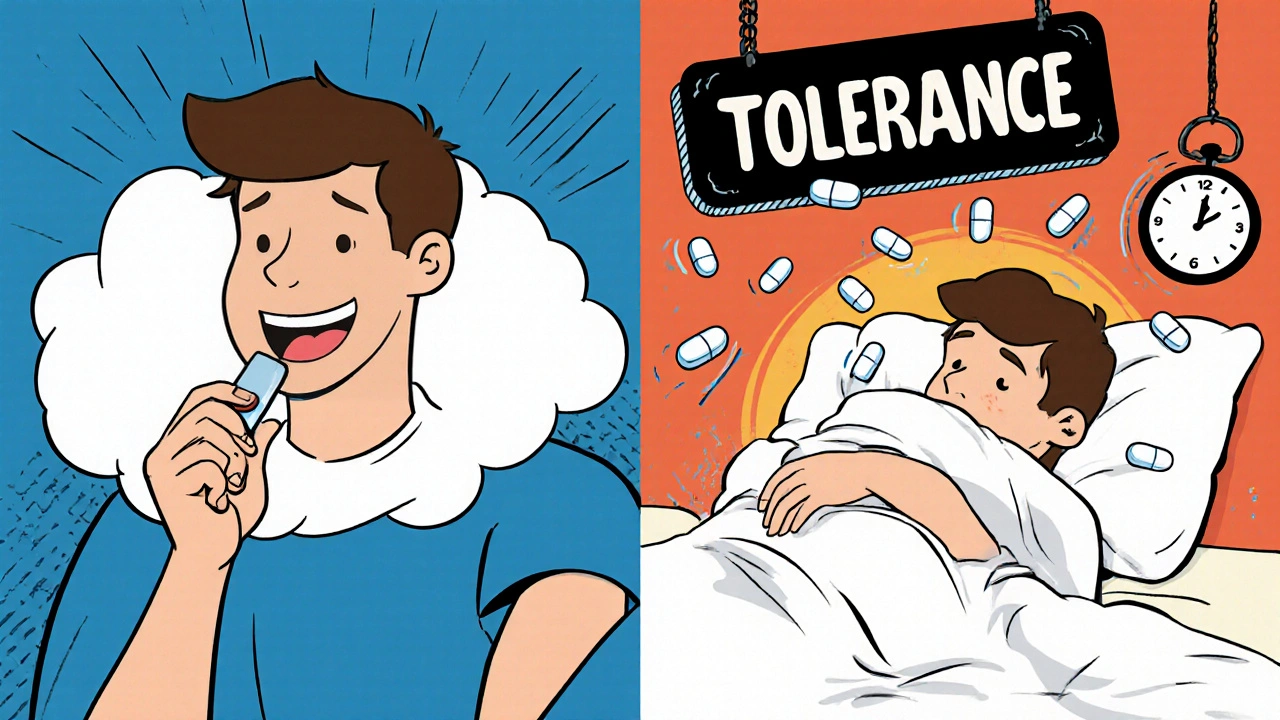
Your body gets used to diphenhydramine. Fast. Within a week of daily use, most people notice it’s not helping as much. That’s tolerance-and it’s your brain adapting to the drug’s presence. So you take more. Or you take it earlier. Or you add another pill. Before you know it, you’re stuck in a cycle: take it to sleep, wake up groggy, feel like you need it again to function.
And here’s what no one tells you: you’re not training your body to sleep better. You’re training it to need a chemical crutch. When you finally stop, the rebound insomnia can be worse than before you started.
Safer Alternatives That Actually Work
You don’t need diphenhydramine to sleep. There are better, safer options-even if they don’t come in a little blue capsule.
Melatonin: The Gentle Reset Button
Melatonin isn’t a sleeping pill. It’s a hormone your body makes naturally to signal bedtime. Taking a low dose (1-3 mg) 30-60 minutes before bed can help reset your internal clock-especially if you’re dealing with jet lag, shift work, or just inconsistent sleep habits. A 2023 meta-analysis found melatonin helped people fall asleep 7 minutes faster and sleep 8 minutes longer on average. No next-day grogginess. No memory fog. No risk of dependency.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
If you want a solution that lasts, CBT-I is the gold standard. It’s not a pill. It’s a structured program-usually 6-8 sessions with a trained therapist-that teaches you how to break the cycle of anxiety around sleep. You learn to associate your bed with rest, not stress. You fix habits that sabotage sleep, like checking the clock at 2 a.m. or lying awake for hours. Studies show 70-80% of people who complete CBT-I see long-term improvement. And the benefits stick around for years, even after treatment ends.
Other OTC Options: Doxylamine and Beyond
Doxylamine (found in Unisom SleepTabs) is another antihistamine, but it’s not much safer than diphenhydramine. It has the same anticholinergic risks and lasts even longer in the body. So skip it. Instead, look at non-histamine options like magnesium glycinate or valerian root-both have modest evidence for helping sleep without the brain fog.
Prescription Alternatives (When Needed)
If your insomnia is severe and ongoing, talk to your doctor. Medications like zolpidem (Ambien) or suvorexant (Belsomra) are approved for short-term use and have fewer cognitive side effects than diphenhydramine. But they’re not for long-term use either. The goal should always be to find the root cause-and fix it without chemicals.
Who Should Avoid Diphenhydramine Completely?
Some people should never take diphenhydramine-even once. This includes:
- Adults over 65
- People with glaucoma
- Men with enlarged prostates
- Anyone with heart rhythm problems
- People taking other sedatives, antidepressants, or anticholinergics
- Children under 12
Even if you’re young and healthy, using it regularly isn’t harmless. It’s a band-aid on a broken system. And band-aids don’t fix broken bones.

What to Do If You’re Already Using It
If you’ve been taking diphenhydramine for more than two weeks, don’t stop cold turkey. That can trigger rebound insomnia or anxiety. Instead:
- Write down why you started using it. Was it stress? Travel? Pain? Anxiety?
- Start cutting back slowly-take half a pill every other night, then every third night.
- Replace it with a non-drug strategy: dim the lights an hour before bed, avoid screens, try a warm bath, or practice deep breathing for 5 minutes.
- Try melatonin (1-3 mg) for a week to see if it helps you fall asleep without the fog.
- Book a chat with your doctor or a sleep specialist. There’s no shame in asking for help.
The goal isn’t to be perfect. It’s to stop relying on something that’s slowly wearing down your brain.
Final Thought: Sleep Isn’t a Problem to Be Fixed-It’s a Habit to Be Rebuilt
We’ve been sold the idea that sleep is something you can buy off a shelf. But real sleep isn’t a chemical trick. It’s a rhythm. It’s consistency. It’s quiet rooms, calm minds, and letting go of the pressure to fall asleep.
Diphenhydramine might give you a few nights of rest. But it steals your clarity, your memory, and your long-term health. There are better ways. They take time. They take patience. But they actually work-and they don’t come with a warning label that says, "May cause dementia."
Is diphenhydramine safe for occasional use?
For healthy adults under 65, occasional use (once or twice a week, for no more than 14 days) is unlikely to cause serious harm. But even then, it’s not ideal. The next-day grogginess, impaired focus, and risk of tolerance make it a poor choice. Safer alternatives like melatonin or better sleep habits are always preferable.
Why is diphenhydramine still sold if it’s so risky?
It’s still sold because it works-for a little while. The FDA classifies it as "Generally Recognized As Safe and Effective" (GRASE) for temporary sleeplessness, based on decades-old data. But newer research shows the risks, especially for older adults, outweigh the benefits. Manufacturers aren’t required to update labels unless the FDA forces them to, and that process is slow. Meanwhile, millions of people keep buying it because it’s cheap and easy to find.
Can diphenhydramine cause addiction?
It’s not addictive in the same way as opioids or benzodiazepines. But you can develop physical dependence. Your body adapts to the drug, so you need more to get the same effect. When you stop, you may experience rebound insomnia, anxiety, or restlessness. That’s not addiction-it’s tolerance. But it’s still dangerous because it traps you in a cycle you can’t easily escape.
What’s the best natural sleep aid?
There’s no single "best" natural aid, but melatonin is the most studied and safest for short-term use. Magnesium glycinate and valerian root have some evidence too, though results vary. The real winner? Consistent sleep hygiene: going to bed and waking up at the same time, avoiding screens before bed, keeping your room cool and dark, and managing stress. These habits fix the root cause-not just the symptom.
Should I talk to my doctor before stopping diphenhydramine?
Yes-if you’ve been using it regularly for more than two weeks. Stopping suddenly can cause rebound insomnia or anxiety. Your doctor can help you taper off safely and suggest alternatives based on your health history. They can also check for underlying issues like sleep apnea, anxiety, or chronic pain that might be causing your insomnia.






Ross Ruprecht
November 22, 2025 AT 13:02Yeah but it works, man. I’ve been taking half a Benadryl for years. Woke up groggy? So what. I sleep. My brain’s fine. Stop scaring people with studies.
Vivian C Martinez
November 22, 2025 AT 15:54I used to rely on this too-until I started waking up feeling like my brain was wrapped in cotton. Switched to 2mg melatonin and a 10-minute breathing routine. No more fog. No more guilt. Just real sleep. You don’t need chemicals to rest.
Bryson Carroll
November 22, 2025 AT 19:42Look I get it you’re all about CBT-I and melatonin like it’s some holy grail but let’s be real most people don’t have the time or patience to sit around breathing and counting sheep. The FDA says it’s okay for occasional use so why are you acting like it’s heroin? You’re not saving anyone you’re just performing moral superiority
Kane Ren
November 23, 2025 AT 18:49My grandma took diphenhydramine for 5 years. She started forgetting where she put her keys… then forgot her own birthday. She’s 78 now and still says she ‘just needed to sleep.’ I wish someone had told her the truth before it was too late. It’s not just grogginess-it’s erosion. Slow. Silent. Deadly.
There’s a better way. It’s not sexy. It’s not quick. But it’s yours. And it lasts.
Karla Morales
November 23, 2025 AT 19:34🚨 PSA: If you’re over 65 and taking this… STOP. 🚨
Also, CBT-I is the only thing that actually works long-term. Not melatonin. Not valerian. Not magnesium. CBT-I. It’s not ‘natural’ so it gets ignored. But it’s evidence-based. And it’s free if your insurance covers it. 📚
Also, diphenhydramine is NOT a sleep aid. It’s a chemical restraint. And we’ve normalized it like it’s tea.
Javier Rain
November 24, 2025 AT 23:10Y’all are overthinking this. I used to take it every night. Got tired of feeling like a zombie. Started walking 20 mins after dinner. No screens after 9. Kept my room at 65°F. Sleep came within 3 days. No pills. No panic. Just discipline.
You don’t need a miracle. You need consistency. And yeah-it’s harder than popping a pill. But you’ll thank yourself at 70.
Laurie Sala
November 25, 2025 AT 08:21...I just... I didn't realize... I've been taking this for over a year... every night... and now I'm scared... I didn't know it could do this to my brain... I feel so stupid... I just wanted to sleep... I didn't know... I'm going to call my doctor tomorrow... please don't judge me... I just... I just wanted to sleep...
...I'm so sorry...
Lisa Detanna
November 25, 2025 AT 21:00In my culture, we use chamomile tea, warm milk with turmeric, and quiet time before bed-no pills. My grandmother lived to 96 and never took a sleep med. She said, ‘Your body knows how to rest. You just have to let it.’
Western medicine pushes quick fixes. But real healing? It’s rhythm. Routine. Respect for your body’s natural clock.
Try it. Not as a replacement. As a return.
Demi-Louise Brown
November 27, 2025 AT 14:16Thank you for this. I’m a nurse. I’ve seen too many elderly patients admitted for confusion after taking OTC sleep aids. It’s not just dementia risk-it’s delirium, falls, hospitalizations. We don’t talk about it enough.
Start small. One change. One night. Dim the lights. No phone. Breathe. You don’t need a pill to rest. You just need permission to try.