PHN Pain Reduction Calculator
Your Current Pain Level
On a scale of 1-10, where 1 is no pain and 10 is worst possible pain, how severe is your pain?
Estimated Pain Reduction
Enter your pain level and select a medication class to see estimated results
When doctors talk about Antidepressants are medications that influence brain chemicals to lift mood and, in some cases, block nerve‑pain signals, they often mention their role in easing postherpetic neuralgia - a lingering nerve‑pain condition that can follow shingles. Treating postherpetic neuralgia pain often involves a mix of drugs, physical therapy, and lifestyle tweaks. This guide breaks down why antidepressants matter, which ones work best, and how to use them safely.
What Is Postherpetic Neuralgia?
Postherpetic neuralgia is persistent nerve pain that lasts more than three months after a shingles outbreak (caused by the varicella‑zoster virus). The virus attacks sensory nerves, and even after the rash clears, the damaged nerves may keep sending pain signals. Symptoms range from burning and stabbing sensations to heightened sensitivity to the lightest touch.
Key facts:
- About 10‑20% of people who get shingles develop PHN.
- Risk increases with age; roughly one‑third of adults over 80 experience it.
- The pain can be constant, intermittent, or triggered by clothing, wind, or temperature changes.
Why Antidepressants Are Considered for PHN
Antidepressants aren’t just mood boosters. Certain classes affect the way nerves process pain. They do this by:
- Blocking the re‑uptake of norepinephrine and serotonin, which dampens pain‑signal amplification.
- Modulating sodium channels in nerve membranes, reducing abnormal firing.
- Improving sleep and mood, which indirectly lowers pain perception.
Because PHN is a type of neuropathic pain, drugs that target neural pathways tend to work better than simple analgesics like acetaminophen.
Antidepressant Classes Used in PHN
Three main families have solid evidence:
- Tricyclic antidepressants (TCAs) - e.g., amitriptyline, nortriptyline, desipramine.
- Serotonin‑norepinephrine reuptake inhibitors (SNRIs) - e.g., duloxetine, venlafaxine.
- Selective serotonin reuptake inhibitors (SSRIs) - e.g., paroxetine, sertraline (used less often, but useful when mood disorders coexist).
TCAs lead the pack, backed by decades of trials. SNRIs are newer, offering similar relief with fewer anticholinergic side effects. SSRIs are usually a secondary choice.
How Each Class Works
TCAs increase levels of norepinephrine and serotonin in the spinal cord, which interferes with pain‑transmission pathways. Their antihistamine and anticholinergic actions can also help patients who have trouble sleeping.
SNRIs have a cleaner side‑effect profile. By inhibiting the re‑uptake of both norepinephrine and serotonin, they boost descending inhibitory pathways that naturally calm pain signals.
SSRIs primarily raise serotonin levels. They are less potent for pain but can be useful if a patient already needs treatment for depression or anxiety.

Evidence Snapshot (2023‑2025)
Recent meta‑analyses give us a clear picture:
- A 2024 Cochrane review of 31 RCTs found that TCAs reduced PHN pain scores by an average of 2.1 points on a 10‑point visual analogue scale (VAS) compared with placebo.
- A 2023 network meta‑analysis ranked duloxetine (an SNRI) second only to amitriptyline in efficacy, with a mean difference of 1.8 VAS points versus placebo.
- SSRIs showed modest benefits (≈0.8 VAS points) and are generally recommended when other indications exist.
Importantly, the benefit‑to‑risk ratio improves when doses start low and titrate slowly.
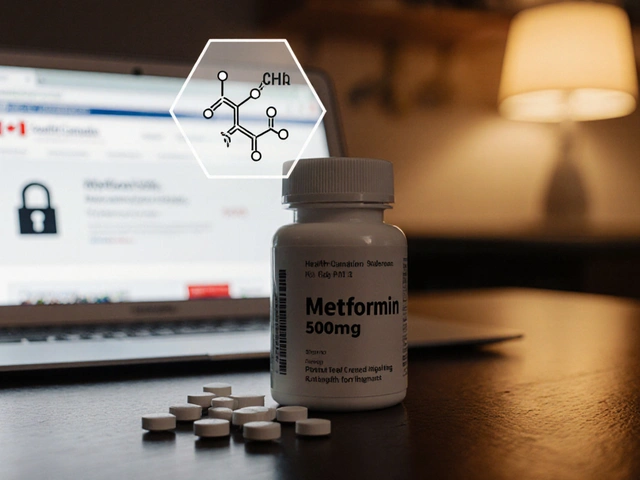
Typical Dosing & Titration
Start low, go slow. Here’s a practical guide:
| Drug | Starting Dose | Target Dose | Typical Side Effects |
|---|---|---|---|
| Amitriptyline | 10mg at bedtime | 25‑75mg nightly | Dry mouth, dizziness, constipation |
| Nortriptyline | 10mg at bedtime | 25‑50mg nightly | Blurred vision, weight gain |
| Duloxetine | 30mg daily | 60mg daily | Nausea, fatigue, insomnia |
| Venlafaxine | 37.5mg daily | 75‑150mg daily | Increased blood pressure, sweating |
| Paroxetine | 10mg daily | 20‑40mg daily | Sexual dysfunction, weight change |
Increase the dose every 3‑7 days if tolerated. Aim for the lowest effective dose to keep side effects in check.
Safety Tips & Contraindications
Antidepressants aren’t risk‑free. Keep these points in mind:
- Heart conditions: TCAs can affect cardiac conduction; avoid in patients with recent MI or uncontrolled arrhythmias.
- Age considerations: Older adults are more sensitive to anticholinergic effects (dry mouth, confusion). Start at half the usual adult dose.
- Drug interactions: Watch for MAO‑inhibitors, certain SSRIs, and grapefruit juice (affects duloxetine metabolism).
- Pregnancy & lactation: TCAs cross the placenta; discuss alternatives with obstetricians.
Regular follow‑up (every 2‑4 weeks initially) helps catch side effects early.
How Antidepressants Compare With Other PHN Options
Other common PHN treatments include gabapentin, pregabalin, lidocaine patches, and capsaicin creams. Below is a quick side‑by‑side view.
| Category | Typical Efficacy (VAS ↓) | Common Side Effects | Cost (US$) |
|---|---|---|---|
| TCAs (e.g., amitriptyline) | ≈2.0 points | Dry mouth, drowsiness | Low |
| SNRIs (e.g., duloxetine) | ≈1.8 points | Nausea, hypertension | Moderate |
| Gabapentin | ≈1.5 points | Somnolence, edema | Low‑Moderate |
| Pregabalin | ≈1.6 points | Dizziness, weight gain | Moderate |
| Lidocaine 5% patch | ≈1.2 points | Skin irritation | High (per patch) |
Antidepressants often win on cost and long‑term adherence, especially when a patient also needs mood support.
Practical Tips for Patients Starting Antidepressants
- Take the first dose at night to harness the sedating effect and reduce daytime drowsiness.
- Keep a pain diary - note intensity, triggers, and any side effects.
- Stay hydrated and chew sugar‑free gum if dry mouth becomes bothersome.
- Don’t stop abruptly. Taper down over at least a week to avoid withdrawal.
- Combine medication with gentle skin care, protective clothing, and low‑impact exercise (e.g., walking) to improve overall well‑being.
When Antidepressants Might Not Be the Right Choice
If a patient has a history of severe cardiac arrhythmia, uncontrolled hypertension, or is on multiple serotonergic drugs, doctors may favor gabapentinoids or topical agents instead. Likewise, if depression isn’t present and side‑effects outweigh benefits, it’s reasonable to discontinue after a trial period of 6‑8 weeks.
Future Directions (2025+)
Research is exploring newer agents that target the same pain pathways with fewer systemic effects. Examples include:
- Novelties like vortioxetine, a multimodal antidepressant showing early promise in small PHN cohorts.
- Combination capsules that pair low‑dose amitriptyline with a topical lidocaine nano‑gel for synergistic effect.
While these are not yet standard care, they indicate a trend toward personalized, multimodal pain control.
Frequently Asked Questions
Can antidepressants cure postherpetic neuralgia?
No. They help reduce pain and improve quality of life, but the underlying nerve damage may remain. Relief usually comes from long‑term use combined with other therapies.
How long should I stay on an antidepressant for PHN?
Most clinicians aim for a minimum of 3‑6 months of stable dosing. If pain returns after stopping, a gradual taper and possible re‑initiation may be needed.
Are there natural alternatives to antidepressants for PHN?
Capsaicin patches, acupuncture, and vitamin B12 supplementation have modest evidence. They are usually adjuncts, not replacements for prescription meds.
What should I do if I experience severe side effects?
Contact your prescriber right away. They may lower the dose, switch to another class, or add a short‑acting medication to manage the side effect.
Is it safe to combine antidepressants with gabapentin?
Yes, many clinicians use a low‑dose TCA plus gabapentin for synergistic relief. Monitor for increased drowsiness and adjust doses accordingly.


Jack Marsh
October 16, 2025 AT 17:25While the article offers a comprehensive overview of antidepressant use in postherpetic neuralgia, it understates the importance of cardiac monitoring when prescribing tricyclic agents. Clinical guidelines emphasize electrocardiographic assessment, particularly for patients with pre‑existing conduction abnormalities. Moreover, the cost analysis omits the long‑term healthcare expenditures associated with adverse events. It would be prudent to incorporate a risk‑benefit discussion that includes cardiac surveillance protocols. In addition, the claim that antidepressants are universally low‑cost neglects price variability across insurance formularies.
Terry Lim
October 19, 2025 AT 00:58Your guide ignores the severe cardiac risks of TCAs.
Cayla Orahood
October 21, 2025 AT 08:32Ever wonder why pharmaceutical giants push these antidepressants so hard? It’s not just about pain relief; it’s a massive profit engine hidden behind the veil of "neuropathic" therapy. The data you cite conveniently glosses over the fact that many studies are funded by drug manufacturers with a vested interest. Don’t be fooled by the glossy efficacy numbers – they often mask selective reporting. Patients end up on chronic medication regimes that keep the cash flowing, while the underlying nerve damage persists. The article also fails to mention the strategic lobbying that keeps these drugs front‑and‑center in guidelines. It’s a classic case of the industry shaping the narrative to suit its bottom line. When you strip away the hype, the reality is far less rosy.
McKenna Baldock
October 23, 2025 AT 16:05Reading through the guide invites a deeper contemplation of how we, as humans, confront chronic suffering. Pain, especially of the neuropathic variety, is not merely a physiological signal but a profound existential burden. When we turn to antidepressants, we are in fact seeking a pharmacological bridge between mind and body, a subtle acknowledgment that emotional state can modulate nociceptive perception. The evidence presented for tricyclic antidepressants is robust, yet one must consider the ethical implications of prescribing a medication primarily designed for mood disorders to treat somatic pain.
First, the pharmacodynamics reveal that TCAs augment norepinephrine and serotonin at the dorsal horn, thereby dampening ascending pain signals. Second, the side‑effect profile, including anticholinergic load, poses particular challenges in geriatric populations where falls and cognitive clouding are already heightened risks. Third, the titration strategy of starting at 10 mg nightly and gradually moving toward 25‑75 mg reflects a cautious optimism that respects the body’s adaptive capacity.
Beyond the biochemistry, there is a philosophical resonance in the notion of “starting low, going slow.” This principle mirrors the Stoic ideal of gradual habituation to hardship, allowing the nervous system to recalibrate without abrupt shock. Moreover, the integration of mood improvement as a therapeutic endpoint underscores the inseparability of affect and sensation.
In practice, the clinician must navigate a delicate balance: harnessing the analgesic potential while vigilantly monitoring for dry mouth, orthostatic hypotension, and cardiac conduction delays. The recommendation to avoid TCAs in patients with recent myocardial infarction is a prudent safeguard, reflecting an awareness of the drug’s intrinsic electrophysiological effects.
Comparatively, SNRIs such as duloxetine present a cleaner side‑effect spectrum, yet their efficacy appears marginally inferior to that of amitriptyline in meta‑analyses. This trade‑off invites a personalized approach, where patient preference, comorbidities, and cost considerations coalesce into a shared decision‑making model.
Looking ahead, the emergence of multimodal agents like vortioxetine hints at a future where we might decouple analgesia from the burdens of traditional antidepressants. Until such innovations become commonplace, the judicious use of existing agents remains a cornerstone of postherpetic neuralgia management. Ultimately, the guide succeeds in distilling complex pharmacology into actionable steps, but it must be read with an appreciation for the broader biopsychosocial tapestry that underlies chronic pain.
Roger Wing
October 25, 2025 AT 23:38People think these drugs are miracle cures but the data is cherry‑picked and the side effects are downplayed the pharma lobby pushes them hard and the guidelines are influenced by money
Andy Williams
October 28, 2025 AT 06:12The dosing table accurately reflects standard practice, though it omits that amitriptyline should be taken with food to mitigate gastrointestinal upset. Nortriptyline’s half‑life warrants cautious titration in renal impairment. Duloxetine requires monitoring of hepatic enzymes if the patient has pre‑existing liver disease. Venlafaxine’s dose‑related rise in blood pressure should be checked each visit. Paroxetine’s interaction with CYP2D6 substrates can lead to elevated plasma levels of concurrent medications.
Mike Brindisi
October 30, 2025 AT 13:45Listen I’ve been on amitriptyline for years and the dry mouth is insane but you can chew sugar‑free gum it helps also keep a water bottle handy it’s not rocket science
Steven Waller
November 1, 2025 AT 21:18It’s valuable to remember that medication is just one piece of the puzzle; integrating gentle exercise, mindfulness, and supportive relationships can amplify the benefits of antidepressants. Patients often report that a regular walking routine, even just 15 minutes a day, improves sleep quality, which in turn reduces pain perception. Encouraging a balanced diet rich in omega‑3 fatty acids may also support nerve health. While pharmacotherapy addresses the biochemical aspect, holistic lifestyle adjustments empower patients to reclaim agency over their recovery.
Puspendra Dubey
November 4, 2025 AT 04:52OMG this article is like a rollercoaster of info 😂 but seriously the way they break down the meds is sooo helpful 8‑) still wish they’d talk more about the emotional roller‑coaster patients feel when dealing with PHN 😭
Shaquel Jackson
November 6, 2025 AT 12:25Interesting read, though I feel a bit overwhelmed by the dosage tables 😐 but overall good job!
Tom Bon
November 8, 2025 AT 19:58The article presents a balanced view of antidepressant therapy, highlighting both efficacy and safety considerations. It appropriately advises clinicians to tailor treatment to individual patient profiles, especially concerning age‑related pharmacodynamics. The inclusion of comparative tables enhances clarity for practitioners seeking quick reference. Overall, it serves as a solid resource for evidence‑based management of postherpetic neuralgia.
Clara Walker
November 11, 2025 AT 03:32Let’s not overlook how pharmaceutical lobbying has shaped the current preference for antidepressants in neuropathic pain. The data often reflects industry‑sponsored trials, which tend to emphasize positive outcomes while downplaying adverse events. National health policies, influenced by these lobbyists, promote these drugs as first‑line therapy, sidelining cheaper non‑pharmacologic options. It’s crucial to remain vigilant about the sources of our evidence.