Many older adults take medications that quietly chip away at their memory and thinking skills - not because the drugs are dangerous on their own, but because of something called anticholinergic burden. This isn’t a single drug or a rare side effect. It’s the combined weight of multiple medications, each blocking a key brain chemical called acetylcholine. Over time, this buildup can accelerate cognitive decline, increase dementia risk, and even change brain structure. And most people - including many doctors - don’t realize it’s happening.
What Exactly Is Anticholinergic Burden?
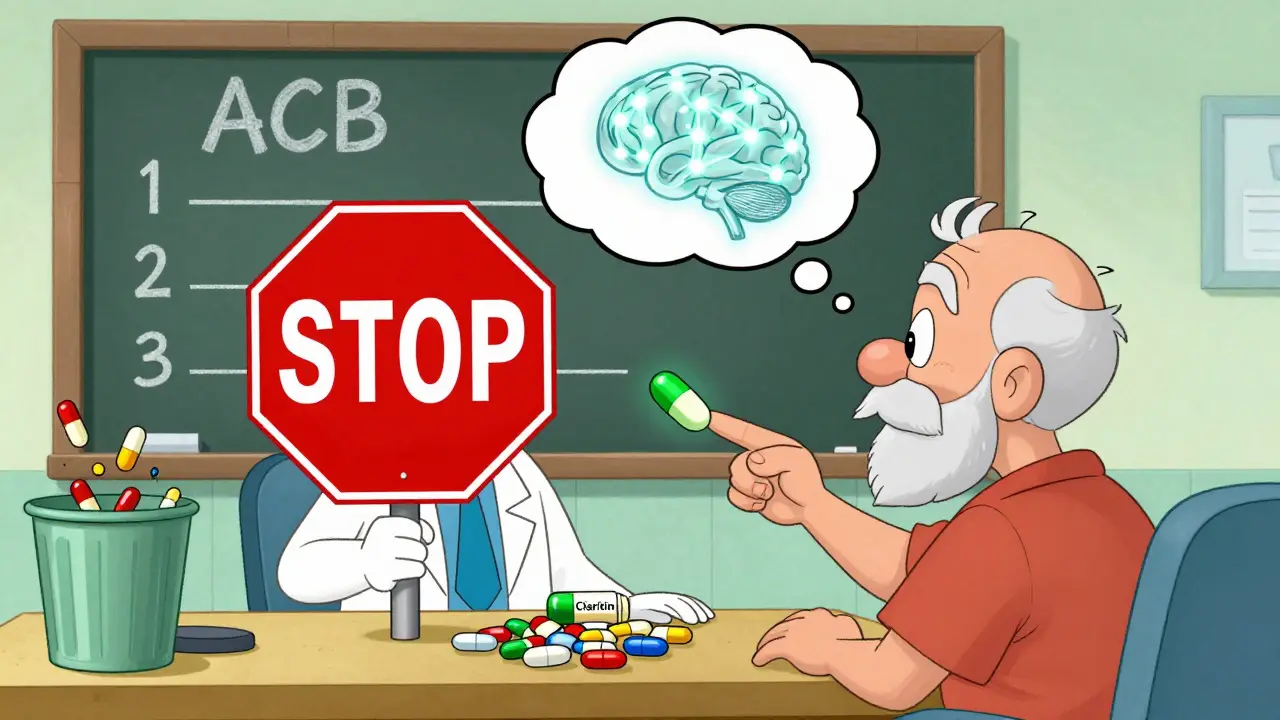
Anticholinergic burden refers to the total effect of drugs that block acetylcholine, a neurotransmitter critical for memory, attention, and learning. When this chemical is suppressed, brain signals slow down. In younger people, the brain often compensates. In older adults, it doesn’t. The damage builds silently. There are three main scales doctors use to measure this burden: the Anticholinergic Cognitive Burden (ACB) scale, the Anticholinergic Risk Scale (ARS), and the Drug Burden Index (DBI). The ACB scale is the most widely used. It rates each medication from 1 to 3:- Level 1 - Mild effect (e.g., cetirizine)
- Level 2 - Moderate effect (e.g., doxepin)
- Level 3 - Strong effect (e.g., diphenhydramine, oxybutynin, amitriptyline)
Which Medications Are the Biggest Culprits?
You might be surprised what’s on this list. These aren’t experimental drugs - they’re staples in medicine cabinets across North America.- Diphenhydramine (Benadryl) - Used for allergies, sleep, or nausea. One 25 mg tablet = ACB Level 3.
- Oxybutynin (Ditropan) - For overactive bladder. Also Level 3. About 1 in 6 high-burden prescriptions in seniors come from this drug.
- Amitriptyline - A tricyclic antidepressant. Often prescribed for nerve pain or depression. Level 3.
- Hydroxyzine - Another antihistamine used for anxiety or itching. Level 2 or 3.
- Chlorpheniramine - Found in many cold and flu mixes. Level 2.
- Scopolamine patches - Used for motion sickness. Level 3.
How Do These Drugs Actually Harm the Brain?
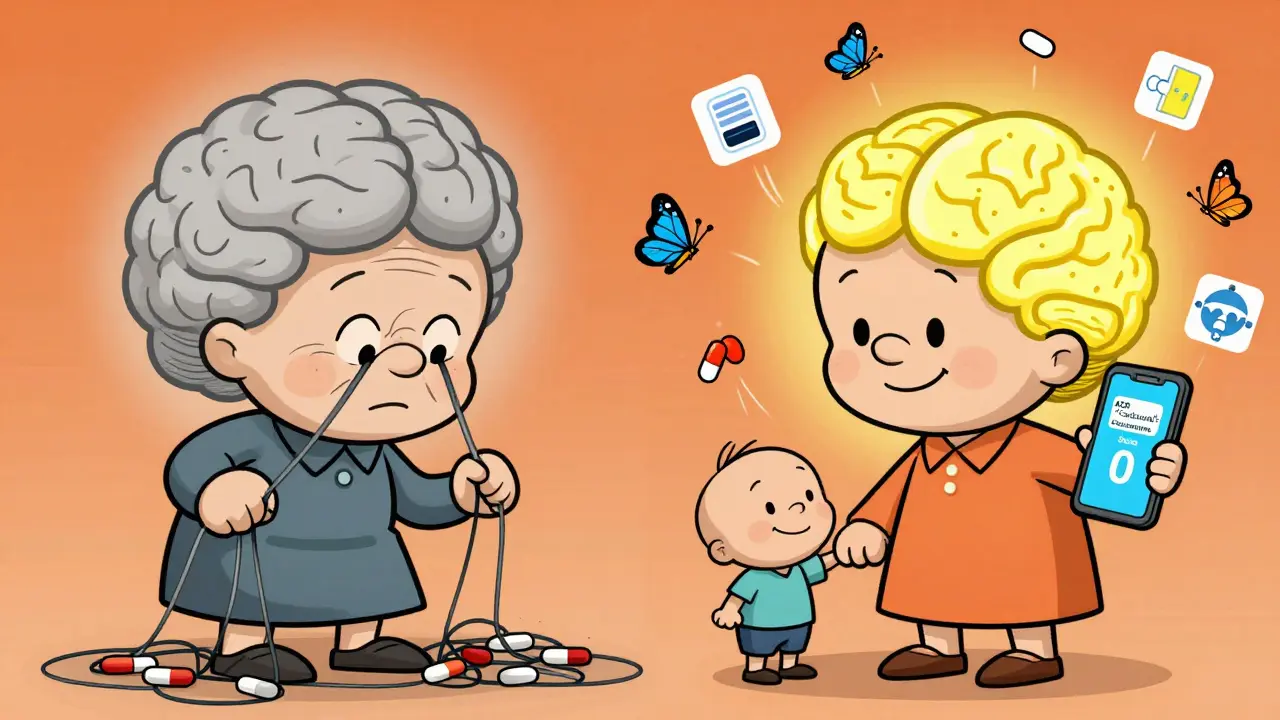
It’s not just about feeling foggy. Brain scans show real, measurable damage. A 2016 study in JAMA Neurology found that older adults taking medications with moderate to high anticholinergic burden had 4% less glucose metabolism in the temporal lobe - the same area that shrinks in early Alzheimer’s. Another study tracked 451 seniors over three years and found they lost brain volume 0.24% faster per year than those not taking these drugs. Why does this happen? Acetylcholine isn’t just for memory. It keeps brain cells alive, helps clear toxins, and supports communication between regions. When you block it, neurons starve. The hippocampus - your brain’s memory center - is especially vulnerable.What Cognitive Skills Are Most Affected?
Not all thinking skills decline equally. Research from the ASPREE trial - which followed nearly 20,000 seniors over nearly five years - showed clear patterns:- Executive function - Planning, organizing, multitasking. Most affected. Each 1-point increase in ACB score led to a 0.15-point drop per year on tests like word fluency.
- Episodic memory - Remembering recent events, names, conversations. Each ACB point caused a 0.08-point annual decline in recall tests.
- Processing speed - How fast you react or solve simple problems. Minimal impact. This suggests the damage isn’t general brain slowdown - it’s targeted.
How Long Does It Take to Cause Real Damage?
The longer you take these drugs, the worse it gets. A landmark 2015 study from the University of Washington found that people who took strong anticholinergics for three years or more had a 54% higher risk of dementia than those who took them for less than three months. Even after stopping, some damage may persist. But here’s the hopeful part: improvement is possible. The DICE trial in 2019 followed 286 older adults who had their anticholinergic meds reduced. After 12 weeks, their Mini-Mental State Exam (MMSE) scores improved by an average of 0.82 points. That’s not a cure - but it’s meaningful. Enough to help someone recognize their grandchild again, or manage their own medications safely.Why Don’t Doctors Always Catch This?
You’d think this would be routine. But it’s not. A 2021 survey of over 1,200 family doctors found that only 37% felt they had enough time during a typical appointment to review all medications for anticholinergic risk. A 2022 study of nursing homes showed that only 39% of residents with high ACB scores had their meds reviewed within three months of being flagged. And patients? A 2021 survey by the National Council on Aging found that 63% of seniors were never told these drugs could hurt their memory. Many assume, “If my doctor prescribed it, it’s safe.” Some of these drugs are sold over the counter. People buy Benadryl for sleep without realizing it’s a Level 3 anticholinergic. Others take oxybutynin for years because no one offered an alternative.What Can You Do?
You don’t have to accept cognitive decline as normal aging. Here’s what works:- Make a full list - Write down every pill, patch, and liquid you take, including OTC and supplements.
- Use the ACB Calculator - The American Geriatrics Society launched a free mobile app in 2024. Just enter your meds, and it gives you a score.
- Ask your doctor these questions:
- Is this medication really necessary?
- Is there a non-anticholinergic alternative?
- Can I try a lower dose or stop it for a few weeks?
- Look for safer options:
- For allergies: Use loratadine (Claritin) or fexofenadine (Allegra) instead of diphenhydramine.
- For overactive bladder: Consider mirabegron (Myrbetriq) or solifenacin (VESIcare) - both have lower brain penetration.
- For depression or nerve pain: Try SSRIs like sertraline or SNRIs like duloxetine instead of amitriptyline.
- Give it time - If you stop an anticholinergic, don’t expect instant results. It takes 4 to 8 weeks for the brain to recover. Some people notice clearer thinking in two weeks.
Real Stories, Real Change
On AgingCare.com, one caregiver wrote: “My mom was confused all the time. She’d forget meals, get lost walking to the bathroom. We blamed dementia. Then we found out she was on oxybutynin for 5 years. We stopped it. Two weeks later, she remembered my name. She started telling stories again.” The FDA has recorded over 1,200 reports of confusion, memory loss, or delirium linked to anticholinergics in seniors between 2018 and 2022. These aren’t rare events. They’re preventable.What’s Changing Now?
The tide is turning. In 2020, the European Medicines Agency banned dimenhydrinate (Dramamine) in dementia patients. In 2022, the FDA required all anticholinergic drugs to add cognitive risk warnings to their labels. Johnson & Johnson pulled its long-acting oxybutynin in 2021. Pfizer pushed out solifenacin, a newer bladder drug with less brain impact. The National Institute on Aging is now funding a $14.7 million study called CHIME, which will test whether reducing anticholinergic burden can delay dementia in 3,500 seniors. Early results are expected by 2027. Experts now say anticholinergic burden is one of the top 10 modifiable risk factors for dementia - potentially responsible for 10 to 15% of cases. That’s more than physical inactivity, and close to smoking.Bottom Line
Your medications shouldn’t steal your memories. If you or a loved one is over 65 and taking any of these drugs - even one - it’s worth asking: Is this really necessary? The good news? You don’t need a specialist. Just a list, a calculator, and the courage to ask your doctor. The brain can recover. Memory can return. And sometimes, the simplest fix is stopping something you didn’t know was hurting you.Can anticholinergic medications cause dementia?
Anticholinergic medications don’t directly cause dementia, but long-term use significantly increases the risk. Studies show people who take strong anticholinergics for three or more years have a 54% higher chance of developing dementia compared to those who use them briefly. This is likely because these drugs reduce activity in brain areas critical for memory and thinking, leading to structural changes over time.
Is Benadryl safe for seniors?
No, Benadryl (diphenhydramine) is not considered safe for regular use in older adults. It’s rated as a Level 3 anticholinergic, meaning it strongly blocks acetylcholine in the brain. It’s linked to confusion, memory loss, and increased dementia risk. Safer alternatives like loratadine (Claritin) or fexofenadine (Allegra) are available for allergies and don’t carry the same cognitive risks.
How do I know if my meds have anticholinergic effects?
Use the free ACB Calculator app from the American Geriatrics Society - just enter your medications and it gives you a score. You can also ask your pharmacist or doctor to review your list. Common culprits include diphenhydramine, oxybutynin, amitriptyline, hydroxyzine, and scopolamine. Even one Level 3 drug can be risky, especially if combined with others.
Can stopping anticholinergic meds improve memory?
Yes, many people see improvement after stopping. In clinical trials, seniors who reduced or eliminated anticholinergic medications showed better memory and thinking scores within 4 to 12 weeks. One study found an average 0.82-point increase on the MMSE cognitive test after 12 weeks. Improvement can be noticeable as early as two weeks, especially if confusion or brain fog was present.
Are there safe alternatives for overactive bladder in seniors?
Yes. Oxybutynin and tolterodine have strong anticholinergic effects. Safer options include mirabegron (Myrbetriq), which works differently and doesn’t cross into the brain, and solifenacin (VESIcare), which has lower central nervous system penetration. Behavioral therapies like timed voiding and pelvic floor exercises can also help reduce symptoms without medication.
How often should seniors have their medications reviewed?
Seniors should have a full medication review at least once a year - and more often if they’ve recently started new drugs, had a hospital stay, or noticed changes in memory or mood. Many experts recommend a review every 6 months for those on multiple medications. Don’t wait for symptoms to appear. Prevention is key.



Bradford Beardall
January 10, 2026 AT 14:57Man, I had no idea Benadryl was this bad for seniors. My grandma takes it every night for sleep. I’m gonna print this out and bring it to her next visit.
McCarthy Halverson
January 11, 2026 AT 06:46Stop the meds. Let the body heal. Simple.
Michael Marchio
January 12, 2026 AT 15:02Let’s be honest - this isn’t about medication safety. It’s about the pharmaceutical industry’s decades-long campaign to keep seniors hooked on pills that barely work anyway. They profit from cognitive decline. They market diphenhydramine like it’s tea. They know the science. They don’t care. And now we’re supposed to trust doctors who got their training from pharma-funded seminars? Please. The system is rigged. The FDA warnings came too late. The real tragedy? It’s all preventable - and nobody’s holding anyone accountable.
Ashlee Montgomery
January 13, 2026 AT 08:53I’ve seen this in my own mother. She was diagnosed with mild cognitive impairment after years on amitriptyline for back pain. We switched her to duloxetine. Within six weeks, she remembered where she put her glasses. Not because she got smarter. Because her brain stopped being suffocated.
lisa Bajram
January 14, 2026 AT 04:10OMG this is LIFE-CHANGING!!! I’ve been begging my mom to stop her oxybutynin for YEARS and she said ‘but the doctor said it’s fine’ - now I’m printing this and taping it to her fridge with a sticky note that says ‘YOUR BRAIN ISN’T A TOILET’ 😭🙌
Christine Milne
January 14, 2026 AT 17:03While I appreciate the sentiment, this article is dangerously oversimplified. The anticholinergic burden scale lacks robust longitudinal validation. The JAMA Neurology study cited had a small sample size and failed to control for polypharmacy confounders. Moreover, the DICE trial’s 0.82-point MMSE improvement is statistically insignificant - less than the margin of error. To suggest that discontinuing these agents reverses cognitive decline is not only premature but potentially harmful. Many elderly patients require these medications for functional independence. Discontinuation without proper alternatives can lead to falls, urinary retention, and depression - all of which accelerate cognitive decline. This is not a public health win. It’s fearmongering dressed as advocacy.
Aurora Memo
January 16, 2026 AT 00:21Thank you for sharing this. I work in senior care and see this every day. The hardest part isn’t the meds - it’s convincing families that ‘it’s just aging’ isn’t true. Sometimes, the bravest thing a person can do is say ‘no’ to a prescription.
Kunal Majumder
January 17, 2026 AT 05:43My uncle in Delhi was on diphenhydramine for sleep for 7 years. He stopped after his grandson showed him this. Now he walks every morning. Talks to everyone. His eyes are clear again. No magic pill. Just stopping the poison.
neeraj maor
January 19, 2026 AT 00:04Who funded this study? Big Pharma wants you to switch to mirabegron - which costs $400/month and is patented by Pfizer. The real agenda? Replace cheap anticholinergics with expensive alternatives. They profit from confusion. They profit from fear. They profit from your ignorance. The FDA? Controlled by lobbyists. The American Geriatrics Society? Funded by drug reps. Even the ACB calculator is a marketing tool. Don’t trust the system. Trust your gut. And if you’re taking anything with ‘-dramine’ or ‘-nium’ - stop everything. Go cold turkey. Your brain will thank you. Or maybe it won’t. Because maybe your memory loss is the system’s way of keeping you from realizing the truth.
Jaqueline santos bau
January 20, 2026 AT 16:17I knew it. I KNEW IT. My husband’s doctor prescribed him amitriptyline for ‘nerve pain’ and suddenly he stopped recognizing his own dog. He forgot my birthday. He cried because he didn’t know why. We didn’t connect the dots until now. I’m so angry. I feel so guilty. Why didn’t anyone warn us? Why is this not on every prescription bottle? This is a national scandal. Someone needs to go to jail for this.
Jake Kelly
January 21, 2026 AT 17:04This is exactly why we need better geriatric training. Not every doctor is bad - but too many are overwhelmed. A simple checklist during med reviews could save thousands of brains. I hope this spreads.
Ritwik Bose
January 22, 2026 AT 23:35Thank you for this deeply thoughtful piece 🙏. As someone from India, I see elderly relatives prescribed diphenhydramine like it’s candy. This is a global issue. We must advocate for awareness - not just in clinics, but in homes, temples, community centers. Knowledge is the first medicine.
Paul Bear
January 23, 2026 AT 07:35While the clinical implications of anticholinergic burden are well-documented in the literature, the article’s conflation of correlation with causation undermines its credibility. The 54% increased dementia risk cited from the University of Washington study is adjusted for age and comorbidities, but not for baseline cognitive reserve, socioeconomic status, or duration of untreated depression - all significant confounders. Furthermore, the ACB scale, while widely adopted, is not a validated biomarker - it’s a heuristic. The 0.24% annual brain volume loss? That’s equivalent to 0.015 mL/year in a 70-year-old - statistically significant, but clinically negligible. To frame this as a ‘red flag’ without acknowledging the risk-benefit calculus of treating nocturia, depression, or chronic pain is irresponsible. The real problem? The absence of shared decision-making, not the drugs themselves.