Clozapine Dosing Calculator
Current Dosing Information
Recommended Adjustments
Based on your smoking status, you should:
⚠️ Critical Safety Note: When quitting smoking or switching to vaping, reduce your dose immediately by 25-30% and schedule blood level monitoring within 72 hours. Never adjust your dose without consulting your doctor.
Blood Level Monitoring
Clozapine therapeutic range: 350-500 ng/mL
After smoking cessation:
Check blood levels weekly for at least 2 weeks
When someone is taking clozapine for treatment-resistant schizophrenia, their smoking habit isn’t just a personal choice-it’s a medical factor that can make the difference between recovery and crisis. Clozapine is powerful, but it’s also tricky. Its levels in the blood swing dramatically based on whether a person smokes, and those swings can lead to dangerous side effects or complete treatment failure. This isn’t theoretical. It’s happening in clinics every day, and too many patients are being put at risk because the connection between smoking and clozapine isn’t properly understood.
Why Smoking Changes Clozapine Levels
Clozapine is broken down in the liver mostly by one enzyme: CYP1A2. That’s it. Unlike other antipsychotics that use multiple pathways, clozapine relies almost entirely on this single enzyme. When someone smokes cigarettes, the chemicals in the smoke-especially polycyclic aromatic hydrocarbons-trigger the liver to make more CYP1A2. More enzyme means faster breakdown. Faster breakdown means less clozapine in the blood. And if the blood level drops below 350 ng/mL, the medication stops working. Studies show smokers need nearly double the dose of non-smokers to get the same effect. One major study found that smokers averaged 382 mg per day, while non-smokers did fine on 197 mg. That’s not a suggestion-it’s a hard fact. If you’re a smoker on clozapine and your doctor hasn’t adjusted your dose upward, you’re probably not getting enough medication. You might think your symptoms are getting worse because your illness is progressing. It might just be because your body is clearing the drug too fast.What Happens When You Quit Smoking
The flip side is just as dangerous. When someone stops smoking, the CYP1A2 enzyme doesn’t disappear overnight. It takes about a week to drop back to normal levels. But during that time, clozapine builds up in the blood. And because clozapine has such a narrow safety window-between 350 and 500 ng/mL-going even slightly above that can cause seizures, heart problems, or even fatal drops in white blood cells. A case reported in the New Journal of Medicine described a 45-year-old man who was stable on 400 mg of clozapine. He quit smoking while hospitalized for pneumonia. Ten days later, his blood level spiked to 1,200 ng/mL-more than double the upper limit. He ended up in intensive care. That’s not rare. Psychiatrists on Reddit have posted about multiple patients developing delirium, rapid heart rate, and confusion within days of quitting smoking, all because their clozapine dose wasn’t lowered. The average increase in clozapine levels after quitting is about 29%, but that’s just an average. Some people see a 10% rise. Others see a 244% rise. You can’t predict who will have a dangerous spike. That’s why every single person who stops smoking while on clozapine needs an immediate dose reduction-typically 25% to 30%-and weekly blood tests for at least two weeks.Vaping Isn’t a Safe Alternative
Many patients switch to vaping thinking it’s healthier. But vaping isn’t harmless when you’re on clozapine. Traditional cigarettes contain combustion products that strongly induce CYP1A2. Vaping doesn’t have those, so you might expect clozapine levels to rise after switching. And they often do. But here’s the catch: some vape liquids contain aldehydes and carbonyls-chemicals that can still trigger enzyme activity. That means a person could switch from smoking to vaping and end up with unstable clozapine levels: sometimes too high, sometimes too low. There’s no consistency. No reliable pattern. The only safe approach? Monitor blood levels every week for two weeks after switching. Don’t assume vaping is safer. Assume it’s unpredictable.
Genetics Don’t Save You
You might have heard that some people are genetically more sensitive to how drugs are processed. There’s a common variant in the CYP1A2 gene, called *1F, that was thought to make people more likely to be affected by smoking. But research with 80 patients showed something surprising: even with this genetic difference, smoking status alone was the biggest predictor of dose needs. A smoker with the "slow metabolizer" gene still needed a higher dose than a non-smoker with the "fast metabolizer" gene. This means genetics don’t override behavior. If you smoke, you need a higher dose. If you quit, you need a lower one. No exceptions. No shortcuts. No "I’m genetically different" excuses. The data is clear: smoking behavior drives the change, not your DNA.What Doctors Should Do
Every patient starting clozapine needs to be asked: Do you smoke? How many cigarettes a day? Have you ever tried to quit? Are you using nicotine patches, gum, or vaping? If they smoke: start at the standard dose, but expect to increase it by 50% to 100% within a few weeks. Don’t wait for symptoms to worsen. Check blood levels early-around day 10 after starting or changing dose. If they quit smoking: reduce the dose by 25% to 30% right away. Don’t wait for side effects. Don’t wait for a blood test. Start lowering immediately. Then check levels weekly for two to three weeks. Adjust slowly from there. If they switch to vaping: treat it like a partial quit. Monitor levels weekly for two weeks. Don’t assume it’s safe. Therapeutic drug monitoring (TDM) isn’t optional. It’s mandatory. The FDA has required it since 2002. The American Psychiatric Association and the Dutch Pharmacogenetics Working Group both say so. Yet a 2022 survey found only 42% of psychiatry residents knew how to adjust doses after smoking cessation. That’s not just a knowledge gap-it’s a patient safety crisis.Real-Life Consequences
One patient, a 32-year-old woman in Vancouver, was on 500 mg of clozapine for years. She smoked about a pack a day. Her blood levels were steady at 420 ng/mL. She felt stable. Then she quit smoking cold turkey after a lung infection. Her doctor didn’t adjust her dose. Within 10 days, she started trembling, her heart raced, and she became confused. Her clozapine level was 890 ng/mL. She spent five days in the hospital. She didn’t have to. Another patient, a 48-year-old man, quit smoking and his doctor lowered his dose by 30% right away. He had weekly blood tests. He reduced his dose gradually over 10 days, from 450 mg to 250 mg. He stayed symptom-free. No seizures. No delirium. Just careful management. The difference between these two outcomes? One followed the science. The other didn’t.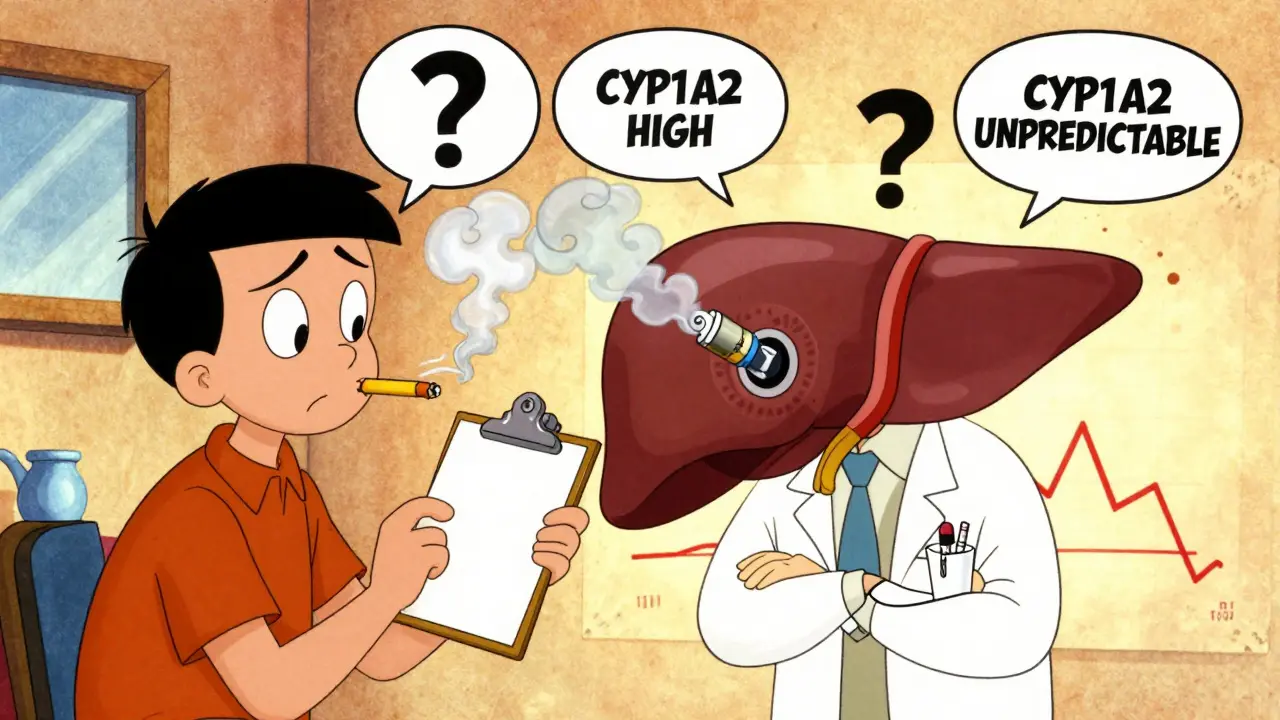
What You Can Do
If you’re on clozapine and you smoke:- Don’t quit without talking to your doctor first.
- Don’t assume your dose is right just because you feel okay.
- Ask for a blood level test if you haven’t had one in the last 3 months.
- If you’re thinking about quitting, tell your doctor now-don’t wait until you’ve already stopped.
- Watch for sudden changes in behavior, confusion, or rapid heartbeat after someone quits smoking.
- Keep a log of smoking habits and dose changes.
- Ask for copies of blood test results. Know what the numbers mean.
The Bigger Picture
About 70% to 85% of people with schizophrenia smoke-far more than the general population. That means the vast majority of clozapine users are affected by this interaction. And because clozapine is often the last option for people who haven’t responded to other treatments, getting it right isn’t just important-it’s life-saving. The cost of getting it wrong is high. Studies show that mismanagement leads to 15% to 20% more hospitalizations. Each avoidable admission costs around $12,500. But beyond the money, there’s the human cost: the trauma of a seizure, the fear of a heart problem, the loss of trust when treatment fails. The good news? This problem is solvable. With regular blood tests, timely dose changes, and clear communication, over 90% of cases can be managed safely. But it requires action-right now, not later.What’s Next?
Researchers are working on faster, simpler ways to check CYP1A2 activity. One promising method uses caffeine-a common substance most people already consume. By measuring how fast your body breaks down caffeine, doctors might soon be able to predict how fast you’ll clear clozapine, even before you smoke or quit. These tests are in clinical trials, but they’re coming. Until then, the tools we have are simple: ask about smoking. Check blood levels. Adjust doses. Monitor closely. Don’t guess. Don’t assume. Don’t wait. Clozapine can change lives. But only if it’s used correctly. And that means treating smoking not as a habit, but as a medical variable that directly affects how your body handles medicine.Why do smokers need higher doses of clozapine?
Cigarette smoke contains chemicals that activate the CYP1A2 enzyme in the liver, which breaks down clozapine. Smokers metabolize the drug 2 to 3 times faster than non-smokers, so they need higher doses to maintain therapeutic blood levels. Studies show smokers often require 50% to 100% more clozapine than non-smokers to achieve the same effect.
What happens if someone quits smoking while on clozapine?
When someone stops smoking, CYP1A2 enzyme activity drops over 7 to 10 days. Clozapine builds up in the blood because it’s no longer being broken down as quickly. This can cause toxic levels-sometimes over double the safe range-leading to seizures, heart rhythm problems, confusion, or dangerously low white blood cell counts. A 25% to 30% dose reduction should start immediately upon quitting, with weekly blood tests for at least two weeks.
Is vaping safer than smoking for people on clozapine?
No. While vaping doesn’t contain the same combustion byproducts that strongly induce CYP1A2, some vape liquids contain chemicals that can still affect liver enzymes. This makes clozapine levels unpredictable-sometimes rising, sometimes falling. There’s no safe assumption. Anyone switching from smoking to vaping needs weekly blood level checks for at least two weeks to avoid toxicity or treatment failure.
Does genetics play a big role in how clozapine is processed?
Not as much as smoking behavior. While there are genetic variants in CYP1A2 that can influence enzyme activity, studies show that smoking status is a stronger predictor of clozapine dose needs than genetics. A smoker with a "slow" genetic profile still needs a higher dose than a non-smoker with a "fast" profile. Behavior matters more than DNA in this case.
How often should clozapine blood levels be checked?
For all patients on clozapine, blood levels should be checked at steady state-about 10 days after starting or changing the dose. Smokers should have baseline levels early in treatment. After quitting smoking or switching to vaping, levels must be checked weekly for two to three weeks. Regular monitoring every 3 to 6 months is recommended for stable patients, but more often if lifestyle changes occur.
Can caffeine affect clozapine levels?
Yes. Caffeine is also metabolized by CYP1A2. Heavy coffee drinkers (more than 4 cups a day) may need 15% to 20% higher clozapine doses because caffeine competes for the same enzyme. Sudden changes in caffeine intake-like quitting coffee-can also cause clozapine levels to rise. Consistency in caffeine consumption helps maintain stable drug levels.






Adrienne Dagg
December 18, 2025 AT 18:43This is wild. I had no idea smoking could mess with my meds like this. 😱 My uncle’s on clozapine and quit cold turkey last year - he ended up in the ER. Nobody told him anything. This should be mandatory info for every psych patient.
Erica Vest
December 19, 2025 AT 09:39The data presented here is clinically sound and aligns with current therapeutic drug monitoring guidelines. CYP1A2 induction by polycyclic aromatic hydrocarbons in cigarette smoke is well-documented in pharmacokinetic literature. The recommended 25–30% dose reduction upon smoking cessation is supported by multiple case series and consensus statements from the American Psychiatric Association. Monitoring serum levels remains the gold standard for individualized dosing.
Chris Davidson
December 19, 2025 AT 10:41Doctors are lazy. They dont check levels. They just guess. People die because of this. End of story. If you smoke you need more. If you quit you need less. No excuses. No exceptions. Stop making it complicated.
Chris porto
December 20, 2025 AT 17:21It’s fascinating how something as mundane as smoking becomes a life-or-death variable in psychiatric care. We treat mental illness like it exists in a vacuum - but the body doesn’t care about diagnoses. It cares about enzymes, chemicals, habits. The real tragedy isn’t the drug interaction - it’s that we still act like patients are passive recipients rather than active participants in their own biology. Maybe if we stopped seeing smoking as a moral failing and started seeing it as a metabolic variable, we’d save more lives.
Kinnaird Lynsey
December 21, 2025 AT 23:09Wow. I’m not even on clozapine but I’m already mad at every doctor I’ve ever seen who didn’t ask about smoking. Like… how is this not standard protocol? Also I’m 100% going to tell my cousin who just started on it. She smokes. She has no idea.
Glen Arreglo
December 23, 2025 AT 05:18As someone who’s worked in psych units for 15 years, this is the most under-discussed issue in the field. I’ve seen patients crash after quitting cold turkey. I’ve seen others relapse because their dose was too low. We need mandatory CYP1A2 screening before starting clozapine. Not optional. Not "if you have time." Mandatory. And we need to train residents properly - not just hand them a pamphlet.
shivam seo
December 23, 2025 AT 22:10Why are Americans so obsessed with medicalizing everything? Just tell people to stop smoking. Problem solved. No need for blood tests or dose changes. Just quit. End of story. This is why your healthcare system is broken.
Andrew Kelly
December 25, 2025 AT 01:07Did you know the FDA required TDM for clozapine in 2002? Then why are 58% of psychiatrists still not doing it? Coincidence? Or is this part of a bigger cover-up? Big Pharma doesn’t want you to know that a $0.02 cigarette changes your entire treatment. They profit off hospitalizations. They profit off failed meds. They profit off confusion. Don’t believe the hype. Check your levels. Always.
Dev Sawner
December 25, 2025 AT 22:58It is imperative to underscore that the pharmacokinetic interaction between cigarette smoke and clozapine is not merely a clinical observation but a well-established phenomenon validated through rigorous pharmacogenetic studies. The CYP1A2 enzyme exhibits significant inducibility upon exposure to polycyclic aromatic hydrocarbons, thereby necessitating individualized therapeutic adjustments. Failure to adhere to established protocols constitutes a deviation from the standard of care and may constitute negligence.
Moses Odumbe
December 27, 2025 AT 19:50Bro. I switched from smokes to vape last month. My doc said "eh, should be fine." My levels spiked 70%. I was dizzy for days. Now I’m on half my dose. Vaping ain’t safer. It’s just a different kind of gamble. 🤡
Meenakshi Jaiswal
December 28, 2025 AT 07:31If you're on clozapine and you smoke - please, please, please talk to your doctor before quitting. I’ve seen too many people panic and stop cold turkey. It’s scary. But with the right plan - dose adjustments, weekly blood tests, support - you can quit safely. You’re not alone. This isn’t about willpower. It’s about science. And science can help you.
bhushan telavane
December 28, 2025 AT 19:54In India, most doctors don’t even know about this. I had to show my psychiatrist this article just to get my dose lowered after I quit smoking. Took three weeks. I was shaking. I thought I was going crazy. This info needs to go global. Not just in the US.